1.3M
Downloads
285
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Thursday Jun 25, 2015
Ep 51 - Day One Round Up (SMACCUS)
Thursday Jun 25, 2015
Thursday Jun 25, 2015
The first day of #smacc15 was amazing. An incredible introduction and an amazing program.

Wednesday Jun 24, 2015
Ep 50 - All in a day's work (SMACC 2015)
Wednesday Jun 24, 2015
Wednesday Jun 24, 2015
In this episode of the St Emlyn's podcast, Simon Carley and Iain Beardsell share insights from the SMACC 2015 conference in Chicago, focusing on the holistic experience of being a clinician. Ian delves into a personal and poignant case involving a 14-year-old boy named Charlie, who tragically died from traumatic injuries. Ian discusses the profound emotional impact this case had on him, the lingering doubts it created, and how it influenced his professional and personal life. This episode highlights the emotional challenges faced by emergency medicine practitioners and underscores the importance of mental resilience, compassionate communication, and self-care.

Wednesday Jun 24, 2015
Ep 49 - SMACC Workshops Review and Pearls
Wednesday Jun 24, 2015
Wednesday Jun 24, 2015
SMACC Chicago: Insights, Learning, and Community at St Emlyn's
The SMACC (Social Media and Critical Care) Conference in Chicago brought together healthcare professionals and thought leaders from around the world. The St Emlyn's team, comprising Iain Beardsell, Simon Carley, Rick Boddy, and Natalie May, participated in various workshops and sessions, sharing their experiences and insights. This blog post captures the essence of the conference, highlighting key learning outcomes and the vibrant community spirit.
Evidence-Based Medicine: From Theory to Practice
Simon Carley kicked off the day with a workshop titled "Gambling with the Evidence," focusing on practical applications of evidence-based medicine (EBM). Unlike traditional EBM sessions that often dwell on statistics and literature reviews, this workshop emphasized how to translate evidence into clinical practice. Simon, alongside Rick Boddy, Rob McSweeney, Ken Milne, and Rory Spiegel, explored how healthcare professionals manage the overwhelming volume of evidence and integrate it into their practice.
Key takeaways included strategies for storing and accessing evidence efficiently, influencing colleagues with evidence-based practices, and the importance of critical skepticism. The workshop stressed the responsibility of individuals to thoroughly understand the evidence before implementing changes in clinical settings. This session underscored the necessity of a balanced approach to adopting new practices, ensuring they are rooted in a comprehensive understanding of available evidence.
FOAM: Creating and Sharing Educational Content
Natalie May joined other prominent figures in the FOAM (Free Open Access Meducation) community for the "Brew Your Own FOAM" session. Alongside Salim Rezé, Rob Rogers, Haney Malamarts, and others, Natalie discussed the creation of blogs, podcasts, and other educational resources. The session, likened to an Apple bar, provided an informal yet informative platform for attendees to engage with experienced content creators.
Participants gained insights into the technical and creative aspects of producing FOAM content. The session encouraged the sharing of knowledge and resources, emphasizing that a diverse range of voices and perspectives enriches the medical community. Natalie highlighted the importance of FOAM in democratizing medical education, making high-quality information accessible to a global audience.
Exploring Chest Pain and Cardiology Pathways
Rick Boddy delved into the nuances of chest pain management and cardiology in his workshops. The morning session on evidence-based medicine included discussions on the values and outcomes in clinical trials, particularly concerning stroke and thrombolysis. Rick emphasized the varying perspectives of patients, doctors, and policymakers, stressing the importance of considering these viewpoints when evaluating clinical outcomes.
The afternoon's emergency cardiology workshop, featuring experts like Steve Smith and Louise Cullen, focused on chest pain pathways. The session covered a range of topics, from ECG interpretation to chest pain algorithms. Rick noted the growing interest in high-sensitivity troponins and the need for tailored chest pain pathways that cater to specific local populations. The discussion also addressed the challenges of implementing standardized pathways and the importance of trusting the evidence.
Getting Creative: Enhancing Communication Skills
Simon Carley also participated in a workshop titled "Getting Creative," which explored creative communication methods in the medical field. The workshop featured three sessions: Michelle Johnson on writing, Grace Slyo on visual presentations, and Rob Rogers on podcasting. Michelle Johnson, a skilled writer, guided participants through the art of crafting compelling narratives, particularly for blog posts. She emphasized the power of language and the importance of clear, concise communication.
Grace Slyo's session focused on improving visual communication, offering tips on graphic design and effective presentation techniques. She provided valuable resources and exercises to help participants enhance their visual storytelling skills. Rob Rogers concluded the workshop with practical advice on creating engaging podcasts, covering everything from content creation to technical aspects. Simon found the workshop incredibly valuable, noting that these skills are essential for effective knowledge dissemination in the medical community.
Pediatric Critical Care: Lessons and Strategies
Natalie May attended the SMACC mini session on pediatric critical care, where experts discussed managing critically ill children in emergency and intensive care settings. The session opened with Fran Lockey and Phil Hyde addressing pediatric airway and breathing management. They emphasized the importance of simple airway maneuvers and two-handed bag-valve-mask ventilation, debunking the myth that intubation is always necessary.
Lisa McQueen provided a poignant presentation on children in shock, referencing the case of Rory Staunton, a child who tragically died from sepsis after being discharged from the emergency department. The session highlighted the critical role of thorough reassessment and face-to-face evaluations in pediatric care. The importance of vigilance in monitoring children's progress before discharge was a key message.
Pre-Hospital Care: Excellence in Action
Iain Beardsell shared his experience from the pre-hospital care workshop, led by Carol Harbig from Greater Sydney Hems. The workshop featured a range of topics and speakers, providing an in-depth look at pre-hospital emergency medicine. The highlight of the day was a presentation by Ashley Leibig, who delivered a powerful talk on the emotional challenges faced by pre-hospital care providers and the importance of peer support.
Iain emphasized the value of visualization and mental rehearsal in preparing for high-stress situations. The workshop underscored the importance of practicing difficult scenarios mentally to ensure readiness when faced with real-life emergencies. This approach helps clinicians develop a clear action plan, reducing the likelihood of hesitation or error during critical moments.
The SMACC Community: Beyond Clinical Knowledge
One of the standout features of the SMACC Conference is its holistic approach to medical education. The conference not only covers clinical and technical topics but also addresses the emotional and psychological aspects of healthcare. Ashley Leibig's talk, reminiscent of Liz Crowe's impactful presentations, reminded attendees of the need for compassion and self-care in a field often dominated by high-stakes decision-making.
The conference provided ample opportunities for networking and community building. The St Emlyn's team noted the importance of connecting with peers, sharing experiences, and learning from each other. The collaborative spirit of the FOAM community was palpable, with participants eager to exchange ideas and support one another in their educational endeavors.
Preparing for the Big Stage: Final Thoughts
As the day drew to a close, the St Emlyn's team prepared for their presentations at the conference. The anticipation and nerves were palpable, reflecting the high regard in which the opportunity to speak at SMACC is held. The team emphasized the importance of thorough preparation, including practicing presentations and ensuring all details are in order.
The St Emlyn's team encouraged attendees and followers to engage with them, highlighting the value of these interactions in enriching the conference experience. They looked forward to meeting new people and deepening connections within the medical community.
Conclusion
The SMACC Conference in Chicago provided a rich and varied learning experience for the St Emlyn's team. From evidence-based medicine to pediatric critical care and pre-hospital medicine, the workshops offered valuable insights and practical knowledge. The conference also underscored the importance of creative communication, emotional resilience, and community support in the medical field.
For those unable to attend, the St Emlyn's team hopes this blog post offers a glimpse into the vibrant and dynamic environment of SMACC. The team is committed to sharing the knowledge and experiences gained at the conference, contributing to the broader medical community's growth and development.
As always, the St Emlyn's team encourages feedback and engagement from their readers. Whether you're interested in evidence-based medicine, FOAM, pediatric care, or any other topic, there's something for everyone in the rich tapestry of SMACC. Stay tuned for more updates and insights as the conference continues to unfold.

Thursday Jun 04, 2015
Ep 48 - Intro to EM: The patient with back pain.
Thursday Jun 04, 2015
Thursday Jun 04, 2015
Managing Back Pain in the Emergency Department: A Comprehensive Overview
In the emergency department (ED), back pain, particularly lower back pain without a traumatic cause, is a common and complex presentation. This condition can range from benign to life-threatening, requiring a thorough and systematic approach to ensure accurate diagnosis and effective management.
The Challenge of Back Pain in Emergency Medicine
Back pain patients often come with preconceived notions, especially when they seek pain relief. However, it's crucial to avoid jumping to conclusions, as back pain can result from various underlying issues, including serious conditions like ruptured abdominal aortic aneurysms (AAA) or infections. Therefore, clinicians should avoid hastily labeling cases as "musculoskeletal" without thorough evaluation.
Key Diagnostic Considerations
1. Broad Differential Diagnosis:
The differential diagnosis should begin with more severe and potentially life-threatening conditions. For example, an AAA can present with subtle back pain, particularly in the elderly, and missing this diagnosis can be catastrophic. Hence, abdominal examinations and bedside ultrasounds are essential tools for detection.
2. Pain Chronology and Characteristics:
Understanding the pain's duration and nature is vital. Chronic pain may suggest long-standing issues, while acute pain can indicate new, potentially severe conditions. Atypical symptoms like pain that worsens at night or at rest, as opposed to musculoskeletal pain that improves with rest, could signal neoplastic or infectious processes.
3. Multi-System Evaluation:
A comprehensive assessment, including vital signs and a review of systems, is critical. For instance, signs like tachycardia, fever, or hypotension can indicate systemic issues such as sepsis. Conditions like pyelonephritis, especially in immunocompromised patients, can manifest as back pain, necessitating a thorough evaluation.
Specific Conditions and Red Flags
Ruptured Abdominal Aortic Aneurysm (AAA):
In elderly patients, AAA must always be considered, especially with sudden onset back pain. This condition can be rapidly fatal, and quick diagnosis via ultrasound is crucial.
Neoplastic Disease:
Symptoms such as unexplained weight loss, persistent night pain, or a history of cancer necessitate evaluation for metastatic disease. Cancers known to metastasize to bone, like breast or lung cancer, may present with back pain, requiring thorough imaging and lab work.
Infectious Causes:
Spinal infections, such as osteomyelitis or epidural abscess, are serious conditions often presenting with back pain. Risk factors include intravenous drug use or immunocompromised states. High suspicion is necessary in patients with concurrent systemic symptoms.
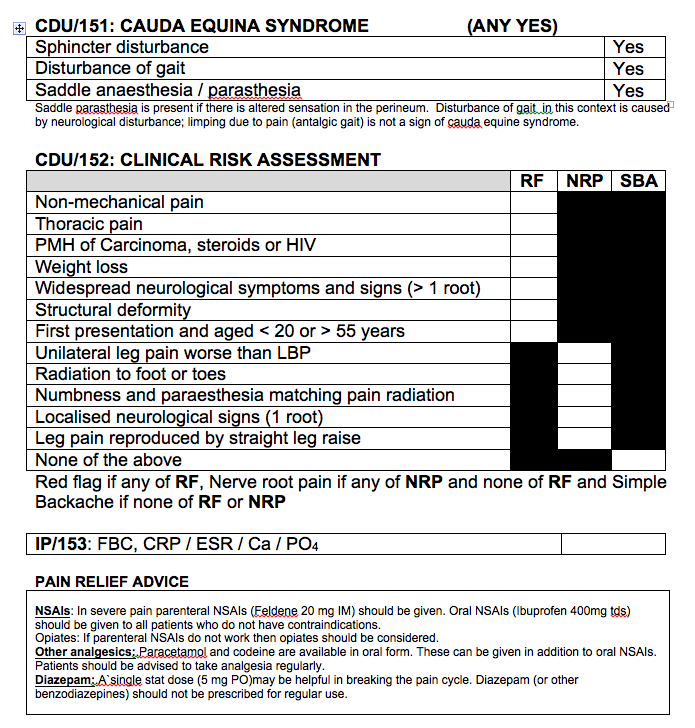
Cauda Equina Syndrome (CES):
CES is a neurosurgical emergency, presenting with symptoms like severe lower back pain, saddle anesthesia, and bowel or bladder dysfunction. A meticulous neurological examination, focusing on lower limb function and perineal sensation, is necessary. MRI is the preferred diagnostic tool, providing detailed images of the spinal cord and nerve roots.
Imaging and Laboratory Tests
Imaging:
Imaging choices should be guided by clinical suspicion. MRI is preferred for evaluating soft tissues, especially in suspected CES cases. For older adults, plain X-rays can reveal fractures but are limited in detecting soft tissue issues. CT scans are useful for complex cases like suspected tumors or infections, while nuclear medicine imaging may detect metastatic lesions or stress fractures.
Laboratory Tests:
Blood tests are essential in cases where red flags suggest systemic involvement. Tests like a full blood count (FBC), inflammatory markers, and bone profiles can provide critical diagnostic information. Elevated inflammatory markers may indicate infection or inflammation, while abnormal calcium levels could suggest a paraneoplastic syndrome.
Management of Non-Specific Back Pain
Once serious conditions are ruled out, management focuses on non-specific, likely musculoskeletal back pain. This involves patient education, mobilization, and appropriate pain management.
Patient Education and Mobilization:
Patients should be informed about the importance of staying active to prevent muscle stiffness and worsening pain. The role of muscle spasm in pain should be explained, and patients encouraged to maintain activity despite discomfort.
Pain Management:
The WHO pain ladder guides pain management, starting with simple analgesics like paracetamol and NSAIDs. For more severe pain, moderate opioids like codeine may be considered. The goal is to provide sufficient pain relief to facilitate mobilization and prevent the development of chronic pain.
Controversial Treatments:
The use of benzodiazepines is controversial. They are not true muscle relaxants but can reduce anxiety and distress, potentially aiding pain management. However, they should be used sparingly and for short periods. The use of gabapentin for acute back pain is also debated, as it is primarily indicated for neuropathic pain.
Chronic Pain Management
For chronic pain patients, management focuses on a multidisciplinary approach, involving pain specialists, physiotherapists, and primary care providers. The goal is to manage the physical, psychological, and social aspects of chronic pain.
Collaborative Care:
Close collaboration with primary care providers ensures consistent messaging and management plans. Pain specialists can offer additional support, especially in complex cases requiring advanced pain management techniques.
Non-Pharmacological Interventions:
Non-pharmacological interventions, such as physical therapy and cognitive-behavioral therapy (CBT), are crucial. These therapies help strengthen muscles, improve posture, and manage the psychological impacts of chronic pain.
Conclusion
In conclusion, managing back pain in the ED requires a comprehensive, systematic approach. Clinicians must prioritize ruling out serious conditions, use appropriate diagnostic tools, and provide effective pain management and patient education. Collaboration with primary care and pain specialists is essential for managing chronic pain, ensuring a holistic approach to patient care. By following these guidelines, healthcare professionals can provide compassionate, evidence-based care, leading to better patient outcomes and a more efficient emergency department.
Red flag symptoms and analgesia advice below.