
1.3M
Downloads
272
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Wednesday Dec 04, 2024
Ep 252 - ECMO in Trauma with Chris Bishop at Tactical Trauma 24
Wednesday Dec 04, 2024
Wednesday Dec 04, 2024
In this episode of the St Emlyn's podcast, hosts Iain Beardsell and Liz Crowe are joined by Chris Bishop, a clinical research fellow at the Centre for Trauma Sciences at Queen Mary University of London. Chris discusses his PhD research on veno-arterial ECMO support for cardiogenic shock following major trauma haemorrhage and explains the principles and applications of ECMO, particularly in trauma patients. The conversation covers the current practices, challenges, and future directions in the use of ECMO for trauma care, including multidisciplinary decision-making, patient selection criteria, and pioneering techniques like selective aortic arch perfusion and emergency preservation and resuscitation.
00:00 Introduction
01:12 Understanding ECMO and Its Applications
02:20 ECMO in Trauma Patients
04:17 Challenges and Resistance in ECMO Adoption
05:36 Current Research and Practices
11:31 Future Directions in Trauma Resuscitation
13:28 Conclusion

Wednesday Nov 06, 2024
Ep 248 - Prehospital eCPR with Alice Hutin at Tactical Trauma 2024
Wednesday Nov 06, 2024
Wednesday Nov 06, 2024
Join Iain Beardsell and Liz Crowe in an engaging discussion with Alice Hutton, an emergency physician from Paris, at Tactical Trauma 24 in Sundsvall, Sweden.
The episode delves into the implementation and logistics of pre-hospital eCPR (Extracorporeal Cardiopulmonary Resuscitation) by SAMU in Paris. Alice shares insights from her PhD research on refractory cardiac arrest and discusses the use of therapeutic hypothermia, including experimental approaches like total liquid ventilation.
Key topics include team composition, decision-making for patient eligibility, real-time management strategies, bypassing traditional emergency rooms for specialized facilities, and the challenges of scene management, family communication, and post-event debriefing.
This conversation offers a comprehensive look at the latest innovations that could transform pre-hospital emergency medical services.
Read more here...
00:00 Introduction and Guest Introduction
01:29 eCPR in Paris: Current Practices
02:35 Dispatch and Response Protocols
03:32 On-Scene Procedures and Challenges
04:23 Decision Making and Scene Management
05:53 Training and Handling Difficult Situations
06:59 Challenges of eCPR Decision-Making
08:07 Importance of Team Debriefing
08:52 Post-Resuscitation Procedures
10:12 Operational Logistics and Success Rates
11:20 Innovative Research in Therapeutic Hypothermia
13:13 Future of Pre-Hospital Cooling Techniques
13:46 Conclusion and Final Thoughts

Sunday Oct 06, 2024
Sunday Oct 06, 2024
In this episode, hosts Iain Beardsell and Simon Carley provide the St Emlyn's podcast blog update for July 2024. They discuss their recent experiences, including Simon's trip to Malaysia for the MRCEM exams and Iain's upcoming attendance at the Tactical Trauma conference in Sweden.
The main topics include a systematic review on the Manchester Acute Coronary Score (MACS) and its application in emergency departments, the potential influence of AI in diagnosing occlusive myocardial infarctions through ECGs, and guidelines for managing non-fatal strangulation cases. Additionally, they touch on the feasibility of using lidocaine patches for elderly patients with rib fractures and the role of partial REBOA in pre-hospital care for exsanguinating subdiaphragmatic haemorrhage.
They also highlight informative segments from the premier conference on pediatric emergency medicine, covering topics such as eating disorders, hybrid closed-loop insulin pumps, and button battery ingestion. Finally, they emphasize the importance of understanding medical statistics and using diagnostic tests effectively in emergency medicine practice.
00:00 Introduction and Summer Updates
00:55 Upcoming Conferences and Events
01:44 Manchester Acute Coronary Score (MACS) Review
05:30 AI in ECG Analysis with Steve Smith
08:18 Non-Fatal Strangulation Awareness
10:45 Reboa: Pre-Hospital Use and Insights
14:11 Pediatric Emergency Medicine Highlights
14:36 Eating Disorders and Diabetes Management
19:00 Lidocaine Patches for Rib Fractures
21:46 Critical Appraisal and Medical Statistics
24:28 Button Battery Ingestion Dangers
26:12 Conclusion and Farewell
Wednesday Jul 10, 2024
Ep 236 - Occlusive Myocardial Infarction, ECGs and AI with Steve Smith
Wednesday Jul 10, 2024
Wednesday Jul 10, 2024
It was a huge pleasure to sit down with Steve Smith, a name synonymous with ECG expertise. Steve, renowned worldwide for his influential ECG blog, has been a pivotal figure in advancing our understanding of ECGs. Many of us have honed our ECG skills thanks to Steve’s insights. I had the opportunity to meet Steve about a decade ago at one of the SMACC conferences. Today, we delve into the fascinating world of occlusive myocardial infarction (OMI) and its comparison to STEMI (ST-elevation myocardial infarction), and explore the promising future of artificial intelligence in ECG interpretation.
In this special episode of the St Emlyn's podcast, we explore the concept of occlusive myocardial infarction (OMI) and its distinctions from ST elevation myocardial infarction (STEMI). Dr. Smith discusses his extensive work and experience in emergency medicine, spanning over three decades, and his development of Dr. Smith's ECG blog. The conversation dives into the limitations of traditional STEMI criteria and the benefits of adopting the OMI paradigm. Additionally, they discuss the revolutionary potential of artificial intelligence in ECG interpretation, particularly through the Queen of Hearts program developed in collaboration with Powerful Medical. Dr. Smith shares compelling studies and real-world applications demonstrating the efficacy of AI in diagnosing ECGs, ultimately offering a promising future for enhanced patient outcomes.
00:00 Introduction
01:43 Steve Smith's Journey in Emergency Medicine and ECGs
02:45 The Evolution of ECG Diagnosis: From STEMI to OMI
03:55 Challenges and Resistance to the OMI Paradigm
07:10 Key Indicators of Occlusive Myocardial Infarction
09:25 The Role of Artificial Intelligence in ECG Diagnosis
11:03 Development and Implementation of the Queen of Hearts AI
14:28 Clinical Studies and Real-World Applications
21:10 Future Prospects and Final Thoughts
A comprehensive blog post with references is available here

Thursday Jun 20, 2024
Ep 233 - Sudden Cardiac Death with Harshil Duptia at PREMIER 2024
Thursday Jun 20, 2024
Thursday Jun 20, 2024
The sudden death of anyone is a tragic event, but even more so a child, particularly when it comes completely unexpectedly. We've all seen stories in the papers or even been involved in caring for these young people. In this podcast Harshil Dhutia talks about the common causes fo sudden cardiac death, and gives a roadmap for the investigation of young people with worrying symptoms and ongoing care for their families.
There are more details in the comprehensive post on the St Emlyn's blog site
This podcast was recorded live at the Hope Church in Winchester as part of the PREMIER conference. We are grateful to the organising team for hosting us and allowing us to use the audio. The PIER and PREMIER websites are full of amazing resources for anyone working in Paediatric Emergency Medicine and we recommend them highly.
The Speaker
Harshil Dhutia is a consultant cardiologist at Glenfield Hospital, University Hospitals of Leicester the lead for inerited cardiac conditions service in the region, providing specialist care for patients with genetic heart diseases and their family members. He is a International Board of Heart Rhythm Examiners certified heart rhythm specialist for all aspects of cardiac device implantation and management including pacemakers, defibrillators and cardiac resynchronisation therapy. He is an expert in sports cardiology and has extensive clinical and research interests in the management of competitive and recreational athletes with cardiovascular disease. He is the medical lead for the Joe Humphries Memorial Trust, a Leicestershire based charity that raises awareness of sudden cardiac death in young people and provides cardiovascular resuscitation and AED training in schools, sports clubs and to members of the community.

Wednesday May 03, 2023
Ep 215 - March 2023 Monthly Round Up
Wednesday May 03, 2023
Wednesday May 03, 2023
Our monthly podcast round up from St Emlyn's Blog. This month Simon and Iain discuss the prehospital use of troponin measurement in the assessment of patients with chest pain and the use of AI in medicine, as well as an update about St Emlyn's WILD.
Please do like and subscribe

Monday Apr 24, 2023
Ep 214 - Shock from St Emlyn’s Medical School
Monday Apr 24, 2023
Monday Apr 24, 2023
This is the first podcast in our new series from St Emlyn's Medical School. They are specifically aimed at healthcare students and focus on the Medical Licensing Assessment (UK) presentations in particular but will be useful wherever you listen in the world.
Each episode has a standard format with a case to set the scene, a set of learning objectives, a discussion, a summary and a case resolution.
There are comprehensive listening notes on the dedicated website, as well as a growing set of other resources.
We hope you enjoy listening. The rest of the podcasts can be found on Spotify, or wherever you get your podcasts.
The music for this series (just as it is for the St Emlyn's Podcast) is composed by Greg Beardsell

Wednesday May 26, 2021
Ep 191 - Adult Congenital Heart Disease in the ED: Part 2
Wednesday May 26, 2021
Wednesday May 26, 2021
This is the second in a two part podcast series discussing Adult Congenital Heart Disease (ACHD) and how these patients may present to the Emergency Department (ED). Dr Sam Fitzsimmons, our guest on the podcast, is a Consultant in Adult Congenital Heart Disease at University Hospital Southampton. There is more information in this blog post.
In this episode we discuss Eisenmenger Syndrome, Transposition of the Great Arteries and Coarctation of the Aorta.
Thursday May 20, 2021
Ep 190 - Adult Congenital Heart Disease in the ED: Part 1
Thursday May 20, 2021
Thursday May 20, 2021
This is the first in a two part podcast series discussing Adult Congenital Heart Disease (ACHD) and how these patients may present to the Emergency Department (ED). Dr Sam Fitzsimmons, our guest on the podcast, is a Consultant in Adult Congenital Heart Disease at University Hospital Southampton. There is more information in this blog post.
Look out for Part 2, which will be released next week, where we discuss Eisenmenger Syndrome, Transposition of the Great Arteries and Coarctation of the Aorta.
Background
With advances in paediatric cardiac surgery, more and more patients with complex congenital heart disease are surviving to adulthood: in the 1950s you might expect a survival rate of about 10%, whereas now this is more like 85%. In fact, there are more patients in the adult congenital heart disease population than there are in the paediatric one (with 2.3 million adults vs 1.9 million children in Europe).
Many patients with Adult Congenital Heart Disease are young and able to live a relatively normal life. This means that they can travel and take part in just the same sort of activities as those without ACHD. They may well turn up in your Emergency Department one day, regardless of whether you are a tertiary centre or a district general hospital (DGH).
They are experts, and know their disease well, but this does not abstain you from a responsibility to know about them too! When these patients become unwell, they can go downhill very fast and you may not have the chance to discuss with them their exact lesion and its management.
The anatomy and physiology of these patients is abnormal, so they may present in atypical ways, and may not respond to usual medical interventions: in fact, some of our usual treatments may even be harmful.
However, starting with our usual 'ABC' approach is by far the best way to go, whilst gathering more information and contacting their specialist centre. Many patients will have their last clinic letter and ECG with them (which will also have the direct dial number of their specialist). And if they, or their relative, say there is something wrong you must believe them and do all you can to make sure they are fully investigated.
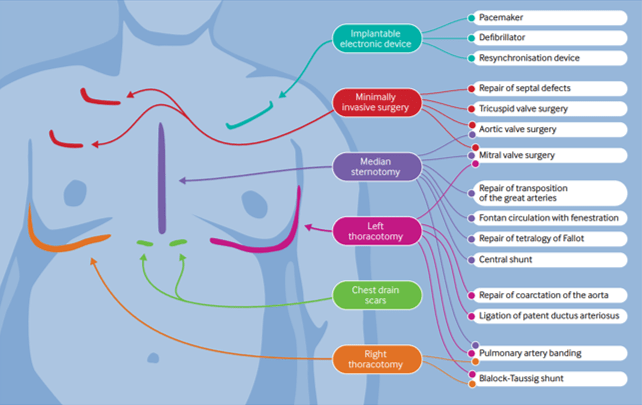
The presence of scars may give you some clues as to the patient's underlying condition and previous surgical repairs. (BMJ 2016; 354: i3905)
A General Approach
- Do your usual ABC assessment.
- Pay particular attention to the respiratory rate - this should be normal.
- Give oxygen if they look unwell.
- They should have a 'normal' blood pressure - any hypotension should be taken as abnormal and investigated.
The Fontan Circulation
This is not a condition in itself, but in fact the resulting circulation after a series of operations that could've been performed due to a number of different underlying conditions:
- Tricuspid Atresia
- Double Inlet Left Ventricle
- Atrio-ventricular Septal Defect – unbalanced
- Pulmonary Atresia
- Hypoplastic Left Heart Syndrome
In essence these patients are born with a single functioning ventricle, that has to be utilised to supply the systemic side of the circulation, whilst the Fontan acts as a passive means of returning blood to the pulmonary circulation.
It was first devised in the early 1970s by Dr Francis Fontan, so the majority of patients with this are in their mid thirties and younger.
Potential reasons for admission to the ED - Fontan circulation
1, Arrythmia
As the patient is entirely dependent on their systemic ventricle to work optimally, any disturbance of the delivery into it is very poorly tolerated. Thus, any arrhythmia is life threatening, even a mild atrial tachycardia.
These patients need to be returned to sinus rhythm as quickly as possible and the recommended method for this is DC cardioversion in expert hands.
Fontan patients have an incredibly fragile circulation and any change in their respiratory physiology can be life threatening, especially if it increases their pulmonary pressures (and thus prevents the passive flow within the Fontan circulation). These patients are not candidates for sedation in the ED and should have an experienced anaesthetist to manage them during the procedure.
Beware if the patient comes in and tells you they are fasted! This means they have been in this situation before and needed DC cardioversion.
2, Haemoptysis
Over time the patient develops venous hypertension within the Fontan connection. This causes the formation of collateral vessels, that may link into the bronchial arterial tree.
If the patient presents in shock treat them as you would any other patient with emergency blood transfusion.
Any haemoptysis, however small, may herald the beginning of a massive bleed. These patients need further investigation, probably a CT chest with contrast. These vessels may then be coiled by interventional radiology.
3, Cyanosis
If the patient has a non fenestrated Fontan they should have normal oxygen saturations. However, if there is a fenestration there will be shunting and therefore a reduction in oxygenation.
For patients this is trade of between being pink or blue, each of which have complications.
Dr Sam Fitzsimmons
Dr Sam Fitzsimmons is a Consultant Cardiologist in Adult Congenital Heart Disease (ACHD) at the University Hospital Southampton, UK. Sam also subspecialises in pulmonary hypertension and maternal cardiology. Working within a tertiary surgical ACHD centre, Sam delivers an ACHD on call service for emergency admissions, inpatient care, routine outpatient follow-up, intra-operative imaging and post-surgical care, as well as specialist clinics in Pulmonary Hypertension and Maternal Cardiology. Sam holds a Honorary Senior Clinical Lecturer post with the University of Southampton as she is passionate about teaching and in particular, she is enthusiastic about helping demystify congenital heart disease for many non-specialist to improve patient care. Sam is well published in peer review journals, cardiology textbooks and specialist guidelines.

Wednesday Apr 24, 2019
Ep 134 - March 2019 Round Up
Wednesday Apr 24, 2019
Wednesday Apr 24, 2019
Highlights from March 2019: Key Insights and Updates
Welcome to the St Emlyn's podcast. I'm Simon Carley and today; I'll be taking you through the highlights from our blog in March 2019. This was a busy month filled with exceptional content, insightful trips, and significant conferences. Let's dive into the details and explore some key topics, starting with adult congenital heart disease, top trauma papers, and the importance of responsible volunteering.
Management of Adult Congenital Heart Disease
March kicked off with an important post on the management of adult congenital heart disease (ACHD). This topic is particularly close to my heart as the hospital I work at is a level two centre for ACHD in the UK. Services have become centralized, and surgical components are now managed at a few specialized centres, with Liverpool being the hub for my region.
Despite this centralization, we still encounter a large population of ACHD patients in our area. These patients often present complex medical histories and unique pathologies that can be challenging to manage in emergency settings. The guidance available typically focuses on chronic and surgical management, but emergency care for these patients requires a different approach.
Common Issues in ACHD Patients
ACHD patients commonly present with dysrhythmias, which can be particularly challenging to manage. Chest pain is also prevalent, although the incidence of ischemic heart disease isn’t significantly higher in ACHD patients, except for those who have undergone certain procedures like the switch operation. Other common issues include:
- Cyanotic patients: Those with single ventricle physiology and right-to-left shunts.
- Endocarditis: A rare but serious complication.
- Non-cardiac problems: Managing ACHD patients with conditions like appendicitis or pneumonia can be complex due to their unique circulatory dynamics.
The bottom line is that these patients often require specialized management strategies. When ACHD patients present with cardiac complications, we consult our local cardiologist or the ACHD centre. However, non-cardiac issues in ACHD patients also warrant discussion with the ACHD centre to ensure comprehensive care.
Key Takeaways for Emergency Physicians
Emergency physicians should familiarize themselves with the unique aspects of Fontan circulation, which relies on venous return based on venous pressure. Aggressive interventions like CPAP, bagging, and diuretics can be detrimental. Understanding these nuances is crucial for providing optimal care.
A Deeper Dive into Fontan Circulation
The Fontan procedure, a surgical intervention for single ventricle defects, creates a unique circulatory system that can be difficult to manage in emergency settings. Unlike normal circulation, Fontan physiology depends heavily on passive blood flow from the veins to the lungs. This means that increasing intrathoracic pressure through methods like CPAP or bagging can reduce cardiac output and worsen the patient's condition.
Fontan patients are particularly vulnerable to fluid shifts and pressures, making careful management of intravenous fluids and medications essential. Understanding these dynamics can be life-saving in the ED. For example, while diuretics might seem a reasonable choice for a patient with fluid overload, they can lead to dangerously low preload and cardiac output in a Fontan patient.
Top Trauma Papers from the Trauma UK Conference
Next up, we revisited some of the top trauma papers presented at the Trauma UK conference. These papers covered a range of topics, from the use of bougies in the ED to bag-mask ventilation during hypertensive resuscitation. Here are some key highlights:
The PAMPer Trial
The PAMPer trial examined the use of prehospital plasma in trauma patients and found significant survival benefits. This trial has important implications for trauma care protocols, emphasizing the potential of early plasma administration to improve outcomes.
The trial showed that administering plasma before hospital arrival can reduce mortality rates in severely injured patients. This finding supports the concept of damage control resuscitation, aiming to stabilize patients early and prevent coagulopathy, acidosis, and hypothermia—the lethal triad in trauma.
Bougie Use in the ED
Another focal point was the utility of bougies in emergency airway management. Evidence suggests that bougies can significantly improve first-pass success rates in difficult intubations, making them a valuable tool in the ED.
A study highlighted at the conference demonstrated that the use of a bougie, even in routine intubations, could increase the success rates for first-pass intubations. This is particularly important in prehospital settings and emergency departments where difficult airways are common.
Late Presenting Head Injury Patients
A paper from Hull explored the management of patients presenting with head injuries more than 24 hours post-injury. The findings indicated that these patients have a significant incidence of important findings on CT scans, suggesting that delayed presentations should not be underestimated.
This study challenges the conventional exclusion of late-presenting head injury patients from acute imaging protocols. It suggests that significant injuries can still be present and warrant immediate attention, even if the patient presents days after the initial trauma.
The Zero Point Survey
The Zero Point Survey, which emphasizes situational awareness, team dynamics, and environmental control before initiating the primary survey, was also highlighted. This approach can significantly enhance resuscitation efforts, ensuring a more organized and effective response.
The Zero Point Survey encourages clinicians to prepare mentally and physically before patient contact. By assessing the situation, assembling the right team, and ensuring the environment is conducive to optimal care, clinicians can improve outcomes and reduce errors in high-stress scenarios.
Responsible Volunteering Overseas
One of the most thought-provoking posts of the month came from Stefan Brisions, discussing the need for responsible volunteering overseas. Volunteering in low and middle-income countries can be incredibly rewarding, but it’s essential to approach it with the right mindset and framework.
The Ethics of Volunteering
Stefan emphasized the importance of volunteering within a system that has sustainability and benefits for all parties involved. There have been concerns about individuals volunteering for personal gain rather than genuine altruism. It’s crucial to ensure that our efforts are focused on creating lasting, positive impacts.
Volunteering should always aim to build local capacity rather than create dependency. This means working with local healthcare providers to enhance their skills and infrastructure, ensuring that the benefits of volunteering continue long after volunteers have left.
Volunteering Responsibly
If you're considering volunteering abroad, it’s vital to engage with established organizations that have a clear mission and ethical framework. This ensures that your contributions are meaningful and aligned with the needs of the local community. Our discussions with experts like Shweta Gidwani, Hooling Harrison, Jennifer Hulls, and Najee Rahman offer valuable insights into this complex issue.
Case Study: Volunteering in South Africa
Kat Evans, who works in Mitchell’s Plain in South Africa, shared her experiences at St Emlyn’s Live. Kat discussed the challenges of working in a resource-limited environment, particularly in managing trauma and toxicology cases.
Her insights into managing trauma in a high-volume, low-resource setting were eye-opening. Kat also shared fascinating details about the use of high doses of atropine for poisoning cases, highlighting the unique medical practices required in such environments.
Kat’s presentation underscored the value of structured volunteer programs that integrate volunteers into local healthcare systems, providing both valuable learning experiences and much-needed support to local healthcare providers.
The Future of SMACC: CODA
March also marked the end of an era with the final SMACC conference in Sydney. SMACC has been a cornerstone for many in the emergency and critical care communities, offering unparalleled opportunities for learning and networking. However, the spirit of SMACC lives on in its successor, CODA.
CODA: A New Beginning
CODA aims to build on SMACC's successes while addressing broader health issues such as vaccination, climate change, and healthcare inequality. The goal is to leverage the engaged community SMACC created to drive meaningful change on a global scale.
CODA plans to tackle these global health issues by bringing together a diverse group of professionals, including those outside the traditional medical fields. This interdisciplinary approach aims to create innovative solutions to some of the world’s most pressing health challenges.
Looking Ahead
While we bid farewell to SMACC, we look forward to the new opportunities CODA will bring. Its emphasis on tackling significant health challenges aligns with the evolving needs of the global healthcare community, promising an exciting future.
What to Expect from CODA
CODA will continue the tradition of high-quality content and dynamic presentations that SMACC was known for. However, it will also incorporate new elements focused on global health advocacy and interdisciplinary collaboration. Expect to see more discussions on how healthcare professionals can contribute to solving broader societal issues.
Additional Highlights from March
Critical Appraisal Nuggets (CANS) on P-values
We also introduced a mini podcast series called Critical Appraisal Nuggets (CANS) focusing on p-values, featuring myself and Rick Body. P-values are a common topic in exams and critical appraisal, and understanding them is crucial for interpreting medical research.
This less-than-ten-minute podcast provides a concise overview of p-values, helping clinicians and students alike grasp this important concept. By demystifying p-values, we aim to enhance our audience's critical appraisal skills, enabling better evidence-based practice.
Dual Coding in Medical Education
Nick Smith, a recent addition to the St Emlyn's team and a brilliant clinical educator, shared insights on dual coding. Dual coding involves using both verbal and visual information to enhance learning and retention.
Nick’s post emphasized how our brains struggle to process multiple streams of information simultaneously. Effective teaching and communication require a balance between verbal explanations and visual aids, ensuring that learners can absorb and retain information without being overwhelmed.
The Impact of Reboa in Trauma Care
Zaf Qasim, a great friend of ours over in the US, examined the impact of Resuscitative Endovascular Balloon Occlusion of the Aorta (Reboa) in trauma care. This post, based on a paper published in JAMA Surgery, analyzed Reboa success rates in civilian trauma using a US database.
The findings suggested that Reboa was associated with higher mortality rates compared to similar patients who did not receive Reboa. This raises important questions about patient selection and the overall benefits of Reboa in trauma care.
Zaf’s post highlighted the need for ongoing research and evidence to determine Reboa's true value. While there are compelling pathophysiological arguments for its use, the clinical outcomes must be scrutinized to ensure it is applied appropriately and effectively.
The Role of Evidence-Based Practice
At St Emlyn's, we prioritize evidence-based practice in all aspects of emergency medicine. The discussions around Reboa, p-values, and dual coding all reinforce the importance of using high-quality evidence to guide clinical decisions and educational strategies.
Final Thoughts
March 2019 was a month of incredible learning and growth. From managing complex ACHD patients to discussing the ethics of volunteering and exploring cutting-edge trauma research, we covered a wide range of topics that are crucial for emergency medicine professionals.
Stay Connected
As we move forward, we encourage you to stay connected with St Emlyn’s for more insights, updates, and discussions. Follow our blog, participate in our events, and join the conversation on social media. Together, we can continue to advance the field of emergency medicine and make a difference in the lives of our patients.
Thank you for joining us this month. Enjoy your practice, and we’ll be back with more great content in April. Have fun, stay safe, and keep learning!

Wednesday Apr 10, 2019
Ep 132 - Aortic Emergencies with George Wills at #stemlynsLIVE
Wednesday Apr 10, 2019
Wednesday Apr 10, 2019
Back in late 2018 we gathered in Manchester for the inaugural #stemlynsLIVE conference. Our friend Dr George Wills gave a great talk on Aortic Emergencies.
All emergency physicians know that it's all to easy to miss an aortic catastrophe. Listen to George's wisdom on common pitfalls and top tips to make you a better emergency clinician.
vb
S
Also check out these excellent #FOAMed resources.
- Subscribe to the blog (look top right for the link)
- Subscribe to our PODCAST on iTunes
- Follow us on twitter @stemlyns
- PLEASE Like us on Facebook
- Find out more about the St.Emlyn’s team
Wednesday Nov 28, 2018
Ep 122 - Beyond ALS with Salim Rezaie at #stemlynsLIVE
Wednesday Nov 28, 2018
Wednesday Nov 28, 2018
Salim Rezaie from the REBEL EM podcast takes us through the optimal management of cardiac arrest and also explores some of the controversies and difficulties that make the difference to our patients.
You can read a lot more about the background to this talk, see the evidence and watch the video on the St Emlyn's site. Just follow this link. https://www.stemlynsblog.org/beyond-acls-salim-rezaie-at-stemlynslive/

Friday May 22, 2015
Ep 47 - Barbra Backus on Risk scores in Acute Coronary syndromes
Friday May 22, 2015
Friday May 22, 2015
Barbra Backus joins Rick Body to discuss the origin, development and future of risk scores for ED patients with possible acute coronary syndromes. Two researchers at the top of their game, and authors of the HEART and MACS scores.

Saturday Jan 24, 2015
Ep 36 - The GoodSAM app with Mark Wilson (LTC 2014)
Saturday Jan 24, 2015
Saturday Jan 24, 2015
Revolutionizing Emergency Medical Response: An Inside Look at the GoodSAM App
Welcome to the St Emlyns blog! Today, we dive deep into an innovation that's poised to transform emergency medical care: the GoodSAM app. I had the privilege of sitting down with Mark Wilson, a consultant neurosurgeon, pre-hospital care practitioner, and the driving force behind this groundbreaking technology. Our conversation took place at the London Trauma Conference, where Mark shared insights into the motivation, development, and future of GoodSAM.
The Birth of GoodSAM: Addressing a Critical Need
Mark Wilson's journey with GoodSAM began through his work with London's Air Ambulance. During his time there, he observed a significant number of patients with head injuries experiencing periods of apnea before medical professionals could arrive. Often, these patients would suffer from hypoxic brain injuries rather than direct trauma to the brain. This observation sparked an idea: what if there was a way to reduce secondary brain injuries by ensuring that airways were kept open during the critical moments before emergency services could reach the patient?
The problem was clear—there simply weren’t enough trained individuals present at the scene of these emergencies to maintain open airways. Inspired by the thought that "you’re never more than five meters away from a spider," Mark and his team theorized that, especially in urban areas like London, you’re likely never more than a few hundred meters away from a trained medical professional.
Developing GoodSAM: From Concept to Reality
Turning this idea into a functioning application required technical expertise and collaboration. Enter Ali Gorgony, a tech developer from Imperial College, who played a crucial role in bringing GoodSAM to life. Together, they conceptualized and built the app, creating a platform that connects individuals in need of immediate medical assistance with nearby responders.
GoodSAM features two primary versions: the Alert app and the Responder app. The Alert app is designed for the general public, while the Responder app is for medical professionals such as doctors, nurses, and paramedics. Once a responder downloads and registers on the app, they are ready to assist in emergencies. The app uses advanced technology to triangulate the responder's location via beacons rather than GPS, ensuring minimal battery drain.
How GoodSAM Works: Saving Lives One Alert at a Time
When someone in distress uses the Alert app, it automatically dials 999 (or the local emergency number in other countries) and simultaneously notifies the three nearest responders. The responder’s phone emits a distinct siren sound, alerting them to the emergency. If they are available to help, they can quickly respond; if not, the next closest responder is notified. This system ensures that someone capable of providing immediate assistance, such as maintaining an open airway or performing CPR, can reach the patient as quickly as possible.
A standout feature of GoodSAM is its defibrillator registry, which currently includes over 12,000 defibrillators. Users can upload pictures of fixed defibrillators in public places, adding to a comprehensive map that responders can access during emergencies.
Ensuring Safety and Reliability: Governance and Verification
The integrity of GoodSAM's responder network is paramount. To ensure that only qualified individuals are registered, responders must upload identification and, if applicable, their GMC number. This information is verified before they are approved to respond to alerts. Additionally, institutions like London’s Air Ambulance and various ambulance services in the UK and Australia can register, allowing their staff to be verified under the institution’s approval.
GoodSAM's governance model is designed to maintain high standards and trust within the community. By verifying the identities and qualifications of responders, the app mitigates the risk of unqualified individuals responding to emergencies.
The Bigger Picture: Integrating with Emergency Services
Mark envisions a future where GoodSAM is fully integrated with emergency services' computer-aided dispatch (CAD) systems. This integration would enable automatic alerts to responders based on 999 calls, even if the GoodSAM Alert app hasn’t been used. This seamless connectivity would ensure even faster response times and potentially save more lives.
Addressing Legal Concerns: The Good Samaritan Act
One of the key concerns for medical professionals considering using the GoodSAM app is indemnity. Mark emphasizes that responding through GoodSAM is akin to performing a Good Samaritan Act. The UK does not currently have a formal Good Samaritan law, unlike parts of the US and Australia, but such legislation is expected to be introduced soon. This law will further protect responders, making it even more challenging for legal action to be taken against them for providing assistance in emergencies.
Sustainability and Social Enterprise: A Model for Good
GoodSAM operates as a not-for-profit social enterprise. Everything discussed so far is free for users—alerting, responding, and usage by ambulance services. The only potential costs arise from integrating with CAD systems, which require development on the part of ambulance services. The altruistic nature of GoodSAM ensures that its primary goal remains to save lives and improve emergency response times.
Spreading the Word: How You Can Help
Mark's call to action is clear: the more people who download and use the GoodSAM app, the greater its impact. He encourages everyone, medical professionals and laypersons alike, to download their respective versions of the app. For responders, having the app on their phone means they can provide critical assistance during emergencies. For the general public, the Alert app can quickly connect them to nearby help, potentially saving lives.
Conclusion: A Community Effort for Better Emergency Care
The development and success of GoodSAM are a testament to the power of community and collaboration. From Mark Wilson's initial observations and ideas to the technical expertise of developers and the support of medical institutions, GoodSAM represents a collective effort to improve emergency medical care. By leveraging technology and crowdsourcing, this innovative app has the potential to make a significant difference in response times and patient outcomes.
If you're inspired by the story of GoodSAM, I urge you to download the app, encourage your friends and family to do the same, and become part of a community dedicated to saving lives. Only good can come from this—literally.

Thursday Oct 23, 2014
Ep 20 - Understanding Troponin Part 3: The NICE guidance.
Thursday Oct 23, 2014
Thursday Oct 23, 2014
Rick and Iain explore how the latest guidance about the use of high sensitivity troponin was developed and how far we can be assured that it is evidence based.
The NICE guidance is available here. http://www.nice.org.uk/guidance/dg15
vb
S
Thursday Aug 07, 2014
Ep 15 - Understanding Troponin - Part 2
Thursday Aug 07, 2014
Thursday Aug 07, 2014
Understanding High Sensitivity Troponins: A Guide for Emergency Physicians
Welcome to the St. Emlyn's podcast. I'm Ian Beardsell and I'm Rick Bodden. This is part two of our troponin special where we delve deeper into high sensitivity troponins (hs-Tn) and their significance in emergency medicine. Today, we'll explore the nuances of hs-Tn assays and how they can enhance our work in the emergency department (ED).
Introduction to High Sensitivity Troponins
High sensitivity troponins (hs-Tn) have transformed how we detect and manage myocardial infarctions (MI) in emergency settings. Unlike traditional assays, hs-Tn tests detect much lower concentrations of troponin, a protein released during myocardial injury, allowing for earlier and more accurate detection of cardiac events.
Analytical Sensitivity vs. Diagnostic Sensitivity
Understanding the difference between analytical and diagnostic sensitivity is crucial. Analytical sensitivity refers to the assay's ability to detect low concentrations of troponin, whereas diagnostic sensitivity relates to the test's performance in diagnosing acute myocardial infarctions (AMI).
Key Points on Analytical Sensitivity:
- Detection Threshold: High sensitivity troponin assays can detect troponin in over 50% of healthy individuals.
- Precision: These assays have a coefficient of variation (CV) of less than 10% at the diagnostic threshold, ensuring consistent results.
Diagnostic Sensitivity:
- Improved Detection: Studies show hs-Tn assays have a higher diagnostic sensitivity (90-92%) compared to older assays (80-85%).
- Early Rule-Outs: This makes hs-Tn particularly valuable for ruling out AMI in patients presenting with chest pain in the ED.
High Sensitivity Troponin Assays: A Closer Look
To illustrate, let's focus on the Roche troponin T high sensitivity assay:
- 99th Percentile Cutoff: 14 nanograms per liter.
- Detection Range: Can detect levels as low as 3 nanograms per liter.
- Higher Readings: It's common for hs-Tn assays to give higher readings than older assays for the same sample, which affects the diagnostic threshold.
The Balance Between Sensitivity and Specificity
While hs-Tn assays improve sensitivity, they may reduce specificity:
- More Positives: Lowering the diagnostic threshold results in more positive results, increasing diagnostic sensitivity but reducing specificity.
- Predictive Value: For example, a positive hs-Tn T result at patient arrival has a specificity around 70% and a positive predictive value of 50%.
Using High Sensitivity Troponins in the Emergency Department
Early Rule-Out Protocols: The most significant advantage of hs-Tn assays is their potential to expedite the rule-out process:
- Zero and Three-Hour Protocols: Studies suggest that hs-Tn assays can effectively rule out AMI with samples taken at 0 and 3 hours after arrival, instead of the traditional 6-hour wait.
- Efficiency: This protocol can significantly speed up patient throughput in the ED, reducing congestion and wait times.
Understanding Deltas: Delta refers to the change in troponin levels between tests:
- Absolute vs. Relative Deltas: Absolute changes (e.g., an increase of 10 nanograms per liter) are often more reliable than relative percentage changes.
- Clinical Context: It's crucial to interpret deltas in the context of the patient's overall clinical picture.
Practical Considerations for Emergency Physicians
Incidental Troponin Elevations: With increased testing at the front door, incidental findings are inevitable:
- Low Pre-Test Probability: In patients with a low pre-test probability of AMI (e.g., mechanical falls), a positive hs-Tn result often does not indicate AMI.
- Clinical Judgment: Consider repeating the test and evaluating the patient's history and clinical presentation before making a decision.
Patients with Comorbidities: Troponin levels can be elevated in patients with various comorbidities:
- Age and Chronic Conditions: Older patients and those with conditions like LV dysfunction may have higher baseline troponin levels.
- Reference Ranges: Use broader reference ranges for patients with comorbidities, as suggested by studies from Paul Collins and colleagues.
Future Directions and Guidelines
Ongoing Research: Research and guidelines on hs-Tn usage are continually evolving:
- NICE Guidelines: Recommendations on using hs-Tn in clinical practice are expected to be published, providing clearer protocols for emergency physicians.
- Early Adoption: As new evidence emerges, early adopters must balance innovation with patient safety.
Point-of-Care Testing: While hs-Tn assays currently require large analyzers, point-of-care testing remains a goal:
- Future Developments: Advances in technology may eventually make hs-Tn testing available at the bedside, further streamlining ED workflows.
Conclusion
High sensitivity troponins represent a significant advancement in the early detection and management of myocardial infarctions in the emergency department. By understanding the nuances of analytical and diagnostic sensitivity, utilizing early rule-out protocols, and interpreting results within the clinical context, emergency physicians can leverage these assays to improve patient care. As always, ongoing research and adherence to evolving guidelines will be essential in optimizing the use of hs-Tn in clinical practice.
We hope this podcast helps you better understand the complexities and advantages of high sensitivity troponins. For more insights and updates, stay tuned to the St. Emlyn's blog and feel free to reach out with your questions and experiences. Together, we can continue to advance emergency medicine for the benefit of our patients.
Sunday Jul 27, 2014
Ep - 11 Understanding Troponin Part 1
Sunday Jul 27, 2014
Sunday Jul 27, 2014
The Ultimate Guide to Understanding Troponins in Emergency Medicine
Welcome to the St. Emlyn's podcast! In this episode, we're exploring the fascinating world of troponins, vital biomarkers essential for diagnosing myocardial injury. Whether you're a seasoned clinician or a medical student, understanding troponins is crucial for effective patient care. We'll cover everything from the basics to advanced concepts, ensuring you have a comprehensive grasp of this critical topic.
What are Troponins?
Troponins are proteins found in muscle tissue, playing a key role in muscle contraction. Often misunderstood as cardiac enzymes, troponins are actually proteins involved in the contractile apparatus within muscle cells. They exist in three forms: Troponin I, Troponin T, and Troponin C, which work together within muscle fibers to regulate muscle contractions.
Why are Troponins Important in Cardiology?
Troponins are crucial biomarkers for diagnosing myocardial injury. When heart muscle is damaged, troponins are released into the bloodstream. This release can occur due to various conditions, including myocardial infarction (heart attack) and other forms of stress on the heart. Measuring troponin levels in the blood helps clinicians determine the extent of myocardial injury and make informed decisions about patient care.
The Difference Between Cardiac and Skeletal Troponins
Troponins are present in both skeletal and cardiac muscle. However, cardiac-specific isoforms of Troponin I and Troponin T can be detected through blood tests, allowing clinicians to specifically identify myocardial damage. This specificity is a significant advancement over previous markers like CK, LDH, and ALT, which were not cardiac-specific and took longer to rise in the bloodstream.
When are Troponins Released into the Blood?
Troponins are released into the bloodstream when there is myocardial injury. This injury can result from various causes, such as acute myocardial infarction, physical stress, or other conditions that strain the heart. Understanding that troponins indicate myocardial injury rather than just myocardial infarction is crucial for accurate diagnosis and treatment.
The Kinetics of Troponin Release
Following myocardial injury, troponin levels typically peak in the blood within 12 to 24 hours. The time it takes for troponin levels to fall depends on several factors, including the severity of the injury, the patient's renal function, and whether there is ongoing troponin release into the blood. For example, patients with significant myocardial infarction might take weeks to clear troponins from their bloodstream, while those with smaller injuries might clear them within a day.
Troponins and Renal Failure
A common question is whether troponin tests are useful in patients with renal failure. The answer is a resounding yes. Although patients with renal failure may have elevated baseline troponin levels due to reduced clearance, troponin testing remains a valuable diagnostic tool. It's essential to interpret these levels in the context of the patient's renal function and look for trends in troponin levels through serial testing.
Understanding Troponin Assays
Troponin tests are immunoassays, which means they use antibodies to target specific parts of the troponin molecule. These antibodies are attached to a signal that emits light, allowing for the quantification of troponin levels in the blood. While lab-based assays are highly accurate, point-of-care testing devices are also available, though they may not be as sensitive or precise as lab tests.
The Role of Point-of-Care Testing
Point-of-care testing devices, such as handheld analyzers, offer quick results and can be used at the bedside. However, they may not match the sensitivity and precision of lab-based assays. Some portable devices provide qualitative results, similar to a home pregnancy test, while others offer quantitative measurements. Clinicians should be aware of these differences and use point-of-care devices appropriately.
Analytical vs. Diagnostic Sensitivity
When discussing troponin assays, it's crucial to differentiate between analytical sensitivity and diagnostic sensitivity. Analytical sensitivity refers to the assay's ability to detect low concentrations of troponin reliably. In contrast, diagnostic sensitivity pertains to the assay's ability to correctly identify patients with the condition being tested for, such as acute myocardial infarction. High-sensitivity troponin assays have improved both analytical and diagnostic sensitivity, enabling earlier and more accurate diagnosis.
Timing of Troponin Testing
In the UK, troponin testing typically starts from the time of symptom onset. This approach differs from other countries where testing begins upon the patient's arrival in the emergency department. The timing of troponin testing is crucial, as early testing can lack sensitivity. Serial sampling over several hours helps ensure accurate diagnosis, with a common practice being to test initially and then again at intervals such as six, ten, or twelve hours after symptom onset.
Interpreting Troponin Levels in Clinical Practice
Interpreting troponin levels requires considering the clinical context and pre-test probability. A positive troponin test in a patient with low pre-test probability of myocardial infarction may not indicate a true positive. Conversely, a negative test in a high-risk patient does not entirely rule out disease, especially if there is potential for a late troponin rise. Clinicians must integrate troponin results with other diagnostic information to make informed decisions.
Troponins in Renal Failure
Patients with renal failure often have elevated baseline troponin levels due to impaired clearance. However, troponin testing remains valuable for diagnosing myocardial injury in these patients. It's essential to understand the baseline level for each patient and focus on changes in troponin levels over time, rather than a single measurement. Serial sampling helps differentiate chronic elevation from acute myocardial injury.
Diagnosing Unstable Angina
It's important to recognize that unstable angina can occur without elevated troponin levels. These patients may not show a rise and fall in troponin but still have significant coronary artery disease that requires attention. Clinical judgment, along with other diagnostic tools like ECG and patient history, is vital in diagnosing and managing unstable angina.
Key Takeaways for Clinicians
- Troponins are proteins involved in muscle contraction and are critical biomarkers for diagnosing myocardial injury.
- Cardiac-specific isoforms of Troponin I and Troponin T are used to detect myocardial damage through blood tests.
- Troponins are released into the blood following myocardial injury, not just myocardial infarction.
- The timing of troponin testing is crucial, with serial sampling providing more accurate results.
- Point-of-care testing devices offer quick results but may lack the sensitivity and precision of lab-based assays.
- Interpreting troponin levels requires considering the clinical context and pre-test probability.
- Troponin testing is valuable in patients with renal failure, focusing on changes in levels over time.
- Unstable angina can occur without elevated troponin levels, requiring careful clinical evaluation.
Conclusion
Understanding troponins and their role in diagnosing myocardial injury is essential for clinicians. From the basics of what troponins are to the nuances of interpreting test results, this knowledge is crucial for providing the best care to patients with suspected cardiac conditions. Stay tuned for our next episode, where we'll delve deeper into high-sensitivity troponin assays and their impact on emergency medicine.
For any questions or further discussion, feel free to comment on the blog post or email us. We're here to help and look forward to continuing this conversation. Until next time, take care and keep learning!
This blog post is brought to you by the team at St. Emlyn's, dedicated to providing high-quality education and resources for emergency medicine professionals.
