
1.3M
Downloads
286
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Saturday Dec 27, 2025
Ep 281 - Best Bits of 2025: Getting Better the Sustainable Way
Saturday Dec 27, 2025
Saturday Dec 27, 2025
January often brings pressure to improve — to fix gaps, sharpen skills, and somehow be better than the year before. Done badly, that drive can become another source of burnout.
This third episode in the Best Bits of 2025 series focuses on how improvement actually works in emergency and acute care — and how to do it in a way that is realistic, sustainable, and kind to the people doing the work.
The clips in this episode are drawn from full St Emlyn’s episodes released during 2025 and reflect some of the most practical conversations about learning, feedback, and professional development from the year.
In this episode, we explore
-
Why clinical skills fade faster than most of us realise — and why teaching is not the same as training
-
How debriefing and video review can drive learning safely, when the culture is right
-
The impact of artificial intelligence and algorithm-driven information on how clinicians learn and make decisions
-
Why conferences, community, and being “in the room” still matter in medical education
This episode is designed for listening on the way to work, on the way home, or during a quieter moment when you’re thinking about how to improve practice without adding more weight.
Featured episodes
Clips in this episode are taken from the following full episodes:
-
Episode 259 — Skills Fade with Nathalie Pattyn (Tactical Trauma 24)
-
Episode 265 — Excellence in Debriefing with Richard Lyon (London Trauma Conference)
-
Episode 267 — Social Media and Artificial Intelligence in Medicine with Peter Brindley
-
Episode 274 — What Medical Conferences Offer in 2025 and How They’ve Changed
All full episodes are available in the podcast feed.
About MedPod Learn
MedPod Learn is a medical podcast player designed to help turn listening into structured learning, with optional tools to support reflection, CPD, and appraisal.
Available on the App Store and Google Play.

Saturday Dec 20, 2025
Ep 279 - Best Bits of 2025: Decisions When It’s Busy
Saturday Dec 20, 2025
Saturday Dec 20, 2025
Emergency medicine strips decision-making back to its essentials when departments are full and time is short.
This first episode in the Best Bits of 2025 series brings together some of the most practically useful moments from the St Emlyn’s podcast this year — focusing on how clinicians make good decisions under pressure, when conditions are far from ideal.
Each clip comes from a full episode released in 2025.
In this episode, we explore:
-
How ten-second triage is designed to work on “worst-day” scenarios, not in textbooks
-
The uncomfortable truth about why procedures sometimes get done — and why that matters
-
Why time, not technique, is often the limiting factor in resuscitative thoracotomy
-
The case for earlier invasive monitoring in the sickest patients
-
Where thinking around double sequential defibrillation may be heading
This episode is designed to be useful on shift, in the car, or during a quiet moment before the next job.
Featured episodes
Clips in this episode are taken from the following full St Emlyn’s episodes:
-
Episode 257 — Ten Second Triage with Sean Brayford-Harris (Tactical Trauma 24)
-
Episode 269 — Monthly Round Up (January 2025): Decision-making and prehospital RSI
-
Episode 270 — Insights on Cannabis Edibles, Pre-Hospital Thoracotomy and more
-
Episode 266 — Monthly Round Up (February 2025): Targeted resuscitation and arterial lines
-
Episode 268 — Top Papers of 2024 from The Big Sick Conference
All full episodes are available in the podcast feed.
About MedPod Learn
MedPod Learn is a clinician-built medical podcast player designed to turn listening into structured learning, with optional MCQs, reflection prompts, and saved activity for appraisal and CPD.
You can find it on the App Store and Google Play.

Wednesday Feb 12, 2025
Ep 260 - Monthly Round Up December 2024 - Chest trauma, IO access, AI and more
Wednesday Feb 12, 2025
Wednesday Feb 12, 2025
In this season-ending episode of the St Emlyn's podcast, Iain Beardsell and Simon Carley come together in Zermatt, Switzerland, to discuss recent studies and updates.
They highlight a randomized control trial on early exercise in blunt chest wall trauma, revealing its limited impact on recovery outcomes. Additionally, they explore the long-term safety of intraosseous access based on new evidence from Denmark.
The episode also provides insights into updated imaging guidelines for paediatric trauma and broad considerations on the growing role of AI in healthcare, especially in emergency settings. There are closing remarks on recent blog posts about toxic alcohol poisoning and the Difficult Airway Society meeting, while looking forward to upcoming conferences in Spain and Vienna.
00:00 Welcome to St Emlyn's Podcast
00:31 Exploring the Big Sick Conference in Zermatt
01:25 Evidence-Based Medicine: Early Exercise in Blunt Chest Wall Trauma
04:30 Intraosseous Access: Long-Term Complications
06:37 Imaging Decisions in Pediatric Trauma
09:17 The Promise and Perils of Artificial Intelligence in Healthcare
13:10 Toxic Alcohol Poisoning: A Critical Review
16:17 Conference Highlights and Future Events
19:19 Season 11 Finale and Looking Ahead to Season 12

Wednesday Jan 29, 2025
Ep 258 - Compassionate Resuscitation with Matt Hooper at LTC
Wednesday Jan 29, 2025
Wednesday Jan 29, 2025
Welcome to our first episode recorded at the London Trauma Conference 2024.
In this episode, hosts Iain Beardsell and Natalie May are joined by Matt Hooper from Adelaide to discuss his unique career path, from emergency medicine to pre-hospital and retrieval medicine, intensive care, and more recently, palliative and end-of-life care.
The conversation centres around the principles of end-of-life care, particularly in acute and traumatic scenarios, and how these can be integrated with life-saving efforts. Key points include the challenges of shifting focus from survival to quality of death, the importance of recognizing and supporting witnesses and caregivers, and the concept of 'compassionate resuscitation.'
Practical tools such as the 'pause' are also explored, aiming to humanize highly charged medical environments and potentially prevent burnout and PTSD among healthcare providers.
00:00 Introduction and Guest Welcome
01:00 Key Messages on Death and Palliative Care
02:12 Challenges in End-of-Life Care
03:20 Improving Quality of Death and Relationships
04:32 Emotional Impact on Care Providers
06:41 Navigating End-of-Life Conversations
12:17 Practical Applications in Intensive Care
16:41 The Pause: A Tool for Reflection 21:58 Conclusion and Final Thoughts
The Guest - Matt Hooper
Matt is an accomplished intensive care specialist with a diverse background in emergency medicine, prehospital & retrieval medicine, and palliative care.
Notable for his leadership in developing critical care service models, he founded South Australia’s MedSTAR Emergency Medical Retrieval Service. He has also co-authored a highly regarded case-based text book and held key teaching and examining roles nationally and internationally in prehospital and retrieval medicine.
With a strong focus on high-performance teams working within high acuity, high consequence environments, Matt's expertise has also extended to human factors in healthcare, cardiothoracic intensive care, ECMO, and clinical ultrasound. More recently however, he has pivoted towards palliative and end of life care, pursuing a Master's degree at Cardiff University and consulting at Mary Potter Hospice in Adelaide. He is passionate about exploring new and innovative ways to prevent potentially avoidable suffering and enhance end of life outcomes for patients in acute care clinical environments.

Wednesday Jan 15, 2025
Wednesday Jan 15, 2025
During Winter's Challenges, Iain Beardsell and Simon Carley reviewed the November 2024 blog posts for St Emlyn's podcast, marking the start of 2025. They discuss the busy state of emergency departments, critical incidents, and the importance of maintaining a learning culture.
They highlight the upcoming Big Sick Conference in Zermatt and the IncrEMentuM in Spain, noting their potential benefits for networking and education.
Simon emphasizes creating a psychologically safe environment and fostering curiosity, growth, and knowledge-sharing among emergency department staff. They also review a range of medical studies, including those on small bore vs. large bore chest tubes for haemothorax, intra-arrest arterial blood pressure monitoring, and the new GLP-1 receptor antagonists for obesity treatment.
Lastly, they address the importance of handling bad behavior in the team and maintaining kindness and professionalism, even during high-stress periods.
00:00 Introduction and New Year Greetings
00:35 Current State of Emergency Departments
01:17 Upcoming Conferences: The Big Sick and IncrEMentuM
03:43 Building a Learning Culture in Emergency Medicine
12:24 Pre-Hospital ECPR and ECMO
13:58 Small Bore vs Large Bore Chest Tubes
17:37 Intra-Arrest Arterial Blood Pressure Monitoring 24:01 New Drugs and Toxicology
24:47 Care in the Hot Zone
27:12 Addressing Bad Behaviour in Emergency Departments
30:42 Conclusion and Future Plans for St Emlyn's

Wednesday Dec 04, 2024
Ep 252 - ECMO in Trauma with Chris Bishop at Tactical Trauma 24
Wednesday Dec 04, 2024
Wednesday Dec 04, 2024
In this episode of the St Emlyn's podcast, hosts Iain Beardsell and Liz Crowe are joined by Chris Bishop, a clinical research fellow at the Centre for Trauma Sciences at Queen Mary University of London. Chris discusses his PhD research on veno-arterial ECMO support for cardiogenic shock following major trauma haemorrhage and explains the principles and applications of ECMO, particularly in trauma patients. The conversation covers the current practices, challenges, and future directions in the use of ECMO for trauma care, including multidisciplinary decision-making, patient selection criteria, and pioneering techniques like selective aortic arch perfusion and emergency preservation and resuscitation.
00:00 Introduction
01:12 Understanding ECMO and Its Applications
02:20 ECMO in Trauma Patients
04:17 Challenges and Resistance in ECMO Adoption
05:36 Current Research and Practices
11:31 Future Directions in Trauma Resuscitation
13:28 Conclusion

Wednesday Oct 30, 2024
Wednesday Oct 30, 2024
In this episode of the St. Emlyn's podcast, hosts Iain Beardsell and Simon Carley share their insights from recent conferences, including Gateshead's RCEM scientific conference, Tactical Trauma 24 in Sweden, and the Premier Conference.
They explore 'Goldilocks moments' for executing life-saving procedures in critical care, emphasizing optimal timing for interventions like thoracotomies. The episode also discusses innovative training methods like shadowboxing to enhance decision-making in high-stress medical scenarios. In addition, they review a significant trial on smoking cessation in emergency departments, highlighting its potential role in broader public health initiatives, including sexual health and HIV screening.
Discussions also cover various pain management strategies, such as the use of intranasal vs. intravenous Ketorolac for renal colic. The hosts critique the traditional peer review process in medical research and advocate for open peer review to support equitable and accessible scientific publishing.
00:00 Introduction and Catching Up
02:07 The Goldilocks Moment in Critical Care
05:25 Training and Decision-Making in Emergency Procedures
07:23 Smoking Cessation in Emergency Departments
10:07 Challenges in Implementing Preventive Health Strategies
10:38 Successful Public Health Projects in Emergency Medicine
11:19 Exploring Alternative Interventions in Emergency Departments
11:52 Highlights from the Premier Conference
12:54 Intranasal Ketorolac for Pain Management
15:46 The Future of Peer Review in Medical Research
20:09 Concluding Thoughts and Upcoming Content
Wednesday Aug 21, 2024
Ep 242 - Prehospital Neuroprotection with Ed Langford at PREMIER 2024
Wednesday Aug 21, 2024
Wednesday Aug 21, 2024
In this episode, we delve into the critical role of neuroprotection in pre-hospital care, particularly in pediatric head injuries. Through a real-life case study of a 13-year-old boy who suffered a traumatic brain injury after being hit by a car, we explore the steps taken by paramedics and critical care teams to stabilize him and prevent further neurological damage. From airway management to advanced interventions, this episode highlights the challenges of pre-hospital neuroprotection and the incredible teamwork that led to the patient’s remarkable recovery.
There is more detail on the full blogpost here.
This podcast was recorded live at the Hope Church in Winchester as part of the PREMIER conference. We are grateful to the organizing team for hosting us and allowing us to use the audio. The PIER and PREMIER websites are full of amazing resources for anyone working in Paediatric Emergency Medicine, and we highly recommend them.
The Speaker
Ed is a Speciality Trainee in Emergency Medicine in Wessex and a trainee Critical Care Practitioner with Dorset and Somerset Air Ambulance. Ed is also the co-founder and Managing Director of Enhanced Care Services, a Southampton-based company delivering enhanced and critical care to the event medical sector, providing frontline ambulance services across Hampshire and clinical education at all levels, employing over 200 clinicians. Ed holds the Diploma in Immediate Medical Care (RCSEd) and, having promised to not take on any more work, is currently undertaking a Masters in Resuscitation, Pre-hospital and Emergency Medicine at QMUL.
Enhanced Care Services
Enhanced Care Services' mission is to provide and influence excellent patient care, irrespective of injury, illness or location, through the delivery of high-quality clinical operations and education. Founded in 2015, ECS now provide frontline ambulance operations across the South, delivers extensive medical cover to some of the most prestigious events across the UK and provides education from its bespoke education centre in Southampton and beyond.

Wednesday Aug 07, 2024
Wednesday Aug 07, 2024
As the UK enjoys its unpredictable summer, with everything from sunshine to hailstorms, we bring you a mix of updates and discussions on emergency medicine, blog content, upcoming conferences, and insightful research reviews. So, whether you're basking in the sun or sheltering from the rain, sit back and enjoy our latest insights into the world of emergency medicine.
In this round-up of Month Year, we talk about a wide range of issues relating to emergency medicine, including nebulised ketamine for analgesia in the ED, risky intubations, presentation skills, more about the DOSE VF trial and analysis of the much-hyped PREOXI trial about preoxygenation before tracheal intubation.
We're excited to announce our participation in two upcoming conferences. The Tactical Trauma Conference in Sweden this October promises to delve into pre-hospital emergency medicine, offering sessions from renowned speakers. It's a fantastic opportunity to learn and network, with flights to Sweden being relatively affordable. The event takes place just north of Stockholm, providing a chance to explore the beautiful city.
In March next year, we look forward to the Incrementum Conference in Murcia, Spain. This is a significant event as emergency medicine has recently been recognized as a specialty in Spain. The conference will feature an impressive lineup of speakers from the FOMED world, including Scott Weingart, Ken Milne, Hany Malamatt, and Slim Resie , among others. Our very own Simon Carly will also be presenting. We'll be there to conduct interviews and gather exclusive content for our listeners.
Thank you for joining us, please do like and subscribe wherever you get our podcasts.

Monday Dec 18, 2023
Monday Dec 18, 2023
In this bumper double edition Simon and Iain chat through all the recent content on the St Emlyn's blog site, including a review of CRYOSTAT-2 and the DAShED study, a review of the new ILCOR guidelines, flow in the ED and why silence might just be the tonic we all need.
All of us at St Emlyn's wish you all, wherever you are on the world a peaceful, happy and restful Christmas.
Please do like and subscribe and get in touch if you'd like to contribute to our ongoing work.

Monday Sep 18, 2023
Ep 223 - July and August 2023 Monthly Round Up
Monday Sep 18, 2023
Monday Sep 18, 2023
After a long, hot and relaxing summer (!) Simon and Iain return with all the content from the St Emlyn's blog in July and August. They discuss four papers in detail, including the ARREST trial about cardiac arrest centres, whether clinical examination can identify life threatening injuries in trauma, the TOP-ART study looking at a novel agent in trauma management and the use of REBOA.
Please do like and subscribe and get in touch if you would like to contribute to the blog site.

Monday Jan 16, 2023
Ep 209 - November and December 2022 Round Up
Monday Jan 16, 2023
Monday Jan 16, 2023
A special double edition covering the blog posts from November and December and more. We discuss evidence based medicine with the DoseVF trial, and more from RECOVERY, discussion about 'what is downtime' and how we organise follow up for patients who don't live in our area and what happened at the amazing London Trauma Conference
We also announced some of the plans for StEmlynsWILD. Look out for booking details and more in the coming weeks.

Tuesday Mar 24, 2020
Ep 157 - ICU for the non-intensivist with Sarah Thorton
Tuesday Mar 24, 2020
Tuesday Mar 24, 2020
Simon chats to Sarah Thornton, consultant anaesthetist, intensivist and head of the NW school of anaesthesia on preparing to work in a critical care unit during the Covid-19 pandemic.

Friday Mar 20, 2020
Ep 156 - February 2020 Round Up
Friday Mar 20, 2020
Friday Mar 20, 2020
Iain and Simon chat about the current Corona pandemic and the blog in Feb 2020.
Iain remains positive, but Simon thinks the glass is half full. Time will tell who is right (though in truth there is a lot of common ground).
S

Wednesday Feb 12, 2020
Ep 154 - January 2020 Round Up
Wednesday Feb 12, 2020
Wednesday Feb 12, 2020
Iain is back on the podcast with Simon to talk through the best of the blog from January 2020.

Saturday Nov 02, 2019
Ep 149 - September 2019 Round Up
Saturday Nov 02, 2019
Saturday Nov 02, 2019
A Month in Review: Key Takeaways from St Emlyn's September 2019 Content
Welcome to a detailed overview of the latest content from St Emlyn's, focusing on the valuable insights and educational resources we shared throughout September 2019. This month’s offerings span a wide range of topics, from the evolving concept of the "resuscitationist" to the increasing challenges posed by decompensated liver disease, and the ongoing development of emergency medicine education. Here’s a look at the most important takeaways.
The Resuscitationist: More Than Just a Title
The term "resuscitationist" has become a buzzword within the emergency medicine (EM) and critical care communities, especially following its emergence from the SMACC (Social Media and Critical Care) conferences. Dan Horner delved into this concept in a recent presentation, sparking a broader discussion about what it truly means to identify as a resuscitationist.
At its core, being a resuscitationist isn’t just about having an interest in the resuscitation room. It requires a blend of sharp clinical skills, deep knowledge of resuscitation science, and the ability to apply evidence-based practices effectively. But beyond technical expertise, leadership and teamwork are crucial. A resuscitationist must excel in managing high-stakes, chaotic situations where decisions are made with limited information and under intense time pressure.
Moreover, Dan highlights the importance of humility and collaboration. The best resuscitationists are those who recognize their own limitations and are skilled at drawing on the strengths of others, whether from different specialties or professions. This collaborative approach not only enhances patient care but also builds stronger, more effective resuscitation teams.
Decompensated Liver Disease: A Growing Concern in the ED
Liver disease is on the rise, particularly due to lifestyle factors like alcohol consumption and obesity. Gareth Roberts tackled this pressing issue in his blog post on decompensated liver disease, which is becoming increasingly common in emergency departments (EDs) across the UK and beyond.
Gareth outlines a comprehensive care bundle designed to manage patients with decompensated liver disease effectively. This bundle includes seven key points:
-
Thorough Investigation: Quick and accurate investigations are essential, particularly for detecting complications like spontaneous bacterial peritonitis (SBP), which can be life-threatening.
-
Infection Management: Aggressive treatment of infections is critical, with a focus on using appropriate antibiotics and monitoring for SBP.
-
Acute Kidney Injury (AKI) and Hyponatremia: These complications are common in liver disease patients and must be managed carefully. Gareth discusses the potential benefits of human albumin in these cases.
-
GI Bleeding: Gastrointestinal bleeding, especially from varices, poses a significant risk. Gareth directs readers to additional resources on St Emlyn’s, including a presentation by Chris Gray on managing GI bleeding.
-
Hepatic Encephalopathy: This condition can severely alter a patient’s mental status and requires careful management. With the increasing prevalence of liver disease, understanding and managing hepatic encephalopathy is more important than ever.
Gareth’s post is a must-read for anyone dealing with liver disease in the ED, providing both practical advice and links to further resources.
Expanding Education: The MSc in Emergency Medicine
Education is a cornerstone of St Emlyn’s, and we’re excited to announce the expansion of the MSc in Emergency Medicine at Manchester Metropolitan University. This program has been running successfully for several years and is now broadening its scope to include paramedics, making it a truly multi-professional and multi-disciplinary course.
The MSc program offers a variety of modules tailored to the specific needs of different healthcare professionals. Whether you’re looking to deepen your clinical knowledge, enhance your leadership skills, or explore new areas of emergency medicine, this program has something to offer. For more details, visit our website or reach out directly.
Supporting St Emlyn’s: Keep Our Content Free and Accessible
St Emlyn’s remains committed to providing free and open-access content to the global emergency medicine community. However, maintaining and expanding our offerings requires resources. If you find value in what we provide, please consider supporting us financially. Even a small contribution can help us continue to deliver high-quality content to healthcare professionals worldwide.
Introducing Coda: The Next Evolution After SMACC
Coda is the latest evolution in the SMACC legacy, aiming to broaden the scope of its predecessor by incorporating a wider range of specialties, including oncology, public health, and surgery. As a member of the Coda executive team, I can attest to the ambitious goals of this new conference series.
Coda retains the clinical excellence that SMACC was known for, but with an added emphasis on advocacy. Each year, Coda will tackle a significant global health issue, with the inaugural theme focusing on climate change and its impact on medical practice.
It’s important to note that while climate change is a key focus, it won’t dominate the entire conference. Only about 25% of the program will be dedicated to this theme, with the remaining 75% featuring the high-quality clinical content you’ve come to expect from SMACC. The first Coda conference is set to take place in Melbourne in 2020, and we encourage you to participate, whether in person or remotely.
The Zero Point Survey: A Game-Changer in Resuscitation
The Zero Point Survey, a concept championed by Cliff Reid, is gaining widespread recognition for its transformative impact on resuscitation practices. The idea shifts the focus of the primary survey in resuscitation from when you first encounter the patient to what you do before you even meet them.
This approach emphasizes the importance of preparation—both mental and environmental. By optimizing everything you can control before the patient arrives, you set the stage for delivering high-quality care when it matters most.
Feedback from the EM community has been overwhelmingly positive, with many clinicians reporting that the Zero Point Survey has changed how they manage the resuscitation room. It’s not just a theoretical concept; it’s a practical tool that’s making a real difference in patient outcomes.
If you’re not yet familiar with the Zero Point Survey, I strongly encourage you to explore the resources available on the St Emlyn’s website, including an excellent video by Cliff Reid that outlines the key elements of this approach.
Looking Ahead: What’s Next for St Emlyn’s?
As we wrap up our review of September’s content, it’s clear that the St Emlyn’s team has been hard at work bringing you the latest in emergency medicine education and clinical practice. But there’s much more to come.
In the coming months, we’ll be covering exciting topics at upcoming conferences, including the ArchiEM conference in Gateshead and the Slovenia ERC conference. These events promise to bring fresh insights and new perspectives that we’ll be sharing with you through our blog posts and podcasts.
In the meantime, keep doing the incredible work you do in emergency medicine. It’s a challenging field, but it’s also incredibly rewarding, and you’re making a difference every day. Thank you for being part of the St Emlyn’s community, and I look forward to continuing this journey with you.
Stay tuned for more great content, and as always, keep pushing the boundaries of what’s possible in emergency care.

Sunday Oct 06, 2019
Ep 147 - August 2019 Round Up
Sunday Oct 06, 2019
Sunday Oct 06, 2019
A Comprehensive Review of St Emlyn’s Blog: August 2019 Highlights
Welcome to St Emlyn’s blog and podcast, where we reflect on the key topics and research from August 2019. In this review, we’ll explore the most impactful discussions and studies, providing valuable insights for emergency medicine professionals. From managing lower GI bleeding and addressing climate change in anaesthesia to examining PTSD in emergency services and the future of diagnostics, this post summarizes essential takeaways that are shaping our field.
Managing Lower GI Bleeding in the Emergency Department
One of the significant topics covered was the management of acute lower gastrointestinal (GI) bleeding, a common but challenging condition in the emergency department (ED). The complexity of managing these cases often lies in determining the correct priority of care, appropriate management strategies, and even the correct speciality for handling these patients.
We reviewed a consensus guideline from the British Society of Gastroenterology and Hepatology, published in Gut, which offers practical recommendations for the diagnosis and management of acute lower GI bleeds. The guideline emphasizes the importance of using stratification tools to distinguish between stable and unstable patients, which can help streamline management in the ED.
For stable patients, the Oakland score is recommended. This scoring system helps identify which patients can be safely managed on an outpatient basis, reducing unnecessary hospital admissions. Conversely, patients with a major bleed should be admitted and scheduled for a colonoscopy at the earliest opportunity. The guideline also highlights the value of CT angiography for hemodynamically unstable patients, a practice increasingly integrated into emergency care.
Transfusion thresholds, set at 70 grams per litre, align with standard practices in other clinical settings, with adjustments for patients with cardiovascular disease. The guideline also recommends having dedicated GI bleed leads within trusts to ensure seamless coordination with emergency services.
Sustainability and Climate Change in Anesthesia
Another crucial discussion from August focused on the environmental impact of healthcare, particularly in anaesthesia. In the UK, healthcare is a significant contributor to climate change, driven by factors like travel, disposable materials, and the use of anaesthetic gases such as nitrous oxide and desflurane.
A key paper by Cliff Shelton and colleagues underscores the need to adopt more sustainable practices in anaesthesia. For example, desflurane is approximately 3,000 times more potent as a greenhouse gas than carbon dioxide. The paper advocates for reducing the use of high-polluting gases and considering greener alternatives where possible.
This shift towards sustainability in healthcare is essential, although challenging, given the nature of medical practice. However, small changes, such as reducing nitrous oxide use in departments where alternatives exist, can collectively make a significant difference. The paper serves as a call to action for healthcare professionals to be more mindful of their environmental impact and to seek sustainable solutions in their practices.
Pre-Hospital Care: Comparing Macintosh and McGrath Laryngoscopes
The debate over the best laryngoscope for pre-hospital rapid sequence intubation (RSI) is ongoing, and in August, we reviewed a study that contributed valuable data to this discussion. Published in Critical Care Medicine, the study compared the Macintosh and McGrath laryngoscopes in pre-hospital settings, involving 514 adult emergency patients.
The study found that both devices were equally effective for pre-hospital RSI. Notably, it also revealed that switching to a different device after a failed intubation attempt was more successful than repeating the attempt with the same device. This finding aligns with the 30-second RSI drills many practitioners use, which advocate for changing the approach after a failed attempt.
These findings have practical implications for both pre-hospital and in-hospital care. In the ED, switching to a video laryngoscope, such as the McGrath, after a failed intubation attempt could improve patient outcomes. As video laryngoscopes become more accessible in emergency departments, integrating them into RSI protocols could be a beneficial strategy.
PTSD in Emergency Services: Rusty Carroll’s Series
Rusty Carroll’s ongoing series on PTSD within the ambulance service continues to be one of the most impactful contributions to the St Emlyn’s blog. The August instalment focused on the aftermath of PTSD, exploring the journey towards understanding what “normal” looks like after such an experience.
Rusty’s candid reflections resonate with many in the emergency services community, highlighting the mental health challenges prevalent in our field. The series has received positive feedback, with many readers finding comfort and validation in Rusty’s experiences.
However, the widespread relatability of this series also underscores a concerning reality: many emergency service professionals are struggling with similar issues. As a community, we need to support one another, promote mental health awareness, and advocate for resources to address the psychological toll of our work. Revisiting Rusty’s previous installments in this series is highly recommended for a deeper understanding of the complex emotions associated with PTSD in emergency services.
The Realities of Packed Red Cell Transfusions
Another fascinating topic from August was the metabolic and biochemical characteristics of packed red cell transfusions, which have significant implications for trauma care in the ED. This discussion was sparked by a conversation on Twitter, leading to critical reflections on the assumptions we hold about blood transfusions.
In trauma care, blood is often regarded as a superior alternative to crystalloids. However, the reality of what we’re transfusing—packed red cells—is quite different from whole blood. A study we reviewed highlighted some surprising statistics about the contents of packed red cells, including a pH of 6.79, a potassium level of 20, and a lactate level of 9.4. These figures reveal that packed red cells are far from the idealized image of whole blood.
The metabolic implications of these characteristics are significant, particularly in the context of massive transfusions. For instance, packed red cells have low levels of 2,3-DPG, which affects their ability to release oxygen to tissues. This raises important questions about how we use blood in trauma resuscitation and whether our current practices are truly optimal.
There’s also an ongoing pre-hospital trial in the UK, known as the RePHILL trial, which is examining the outcomes of patients randomized to receive either blood or no blood in pre-hospital settings. The results of this trial are eagerly anticipated and could challenge the assumption that blood is always better. This could lead to more nuanced transfusion practices in the future.
The Future of Diagnostics: Insights from Rick Body
Finally, we explored the future of diagnostics with insights from Rick Body. His presentation, originally given at the St Emlyn’s Live conference, offers a compelling vision of where diagnostics in the ED is heading. With the rise of machine learning, artificial intelligence (AI), and personalized diagnostics, the landscape of emergency medicine is rapidly evolving.
These technologies are already being integrated into diagnostic processes, but they bring new challenges. The data generated by AI and machine learning can be complex, requiring a shift in how we interpret diagnostic results. We must move away from binary thinking and embrace a more nuanced understanding that includes probabilities, uncertainties, and complexities.
As emergency medicine professionals, we need to prepare for this shift by engaging with these new technologies and incorporating them into our clinical practice. The future of diagnostics is exciting, but it will require ongoing education and adaptation to fully harness its potential.
Conclusion
August 2019 was a month rich with insightful discussions and important research that continue to influence our practice in emergency medicine. From managing lower GI bleeding and the environmental impact of anaesthesia to the complexities of blood transfusions and the future of diagnostics, these topics highlight the diverse challenges and opportunities we face in the ED.
The St Emlyn’s blog and podcast aim to keep you informed and engaged with the latest developments in our field. This review has provided valuable insights that can be applied in your practice, helping you stay ahead in the ever-evolving landscape of emergency medicine. Stay tuned for more updates, and as always, feel free to share your thoughts and experiences with us. Until next time, take care and continue to push the boundaries of what’s possible in emergency medicine.

Saturday Oct 05, 2019
Ep 146 - European Resus Council meeting Slovenia 2019
Saturday Oct 05, 2019
Saturday Oct 05, 2019
A vox pop round up of the best of the ERC19 conference in Slovenia.

Friday Sep 27, 2019
Ep 145 - The UK Resuscitationist with Dan Horner at #stemlynsLIVE
Friday Sep 27, 2019
Friday Sep 27, 2019
Our latest podcast from the #stemlynsLIVE conference last year. Dan Horner talks on the concept and potential role of the UK Resuscitationist.
Tuesday Sep 10, 2019
Ep 144 - July 2019 Round Up
Tuesday Sep 10, 2019
Tuesday Sep 10, 2019
St Emlyn’s July 2019: Key Highlights
Welcome back to St Emlyn’s, where we continue to share the latest insights, discussions, and advancements in emergency medicine. July 2019 was particularly rich in content, covering a wide range of topics from practical clinical advice to deeper reflections on the ethics and philosophy of emergency medicine. Here, we summarize the key points from the month’s posts, optimized for clarity and relevance.
Upcoming Events: Resuscitology Course and MSc in Emergency Medicine
Before diving into the content highlights, there are two important announcements:
Resuscitology Course – December 2019
On December 14th, 2019, the Resuscitology course will be held in Manchester. This course, led by Cliff Reid, offers an in-depth exploration of why certain resuscitation techniques work and how they can be improved in high-stakes scenarios. This is a must-attend for anyone involved in emergency or critical care. Registration details are available on our blog.
MSc in Emergency Medicine – 2019-2020 Cohort
Recruitment is now open for the 2019-2020 cohort of the MSc in Emergency Medicine. This three-year online program, available to both doctors and nurses, offers an advanced curriculum in emergency medicine. Alumni like Janus Bae, Alan Grace, and Natalie May have found it immensely beneficial. By 2020, we hope to extend the program to paramedics as well, broadening its reach and impact.
July 2019 Blog Highlights
This month’s content ranged from clinical insights and research updates to philosophical discussions about the practice of emergency medicine.
Disaster Medicine in Pakistan: Lessons Learned
Zaf Kasim, now practicing in the United States, and Rashid Akhil from Pakistan collaborated on a blog post discussing the management of natural disasters, terrorist attacks, and major incidents in Pakistan. Zaf, who trained with us in Verchester, has become an authority in endovascular resuscitation, REBOA, and ECMO.
This post sheds light on the expertise developed by medical professionals in Pakistan, particularly in response to large-scale disasters like the 2005 Kashmir earthquake. It’s a crucial read for anyone interested in global health or disaster medicine, as it demonstrates how effective disaster response systems can be developed even in resource-limited settings.
Managing Major GI Hemorrhage: Practical Insights
Chris Gray revisited a talk he gave at the St Emlyn’s Live Conference, focusing on the challenges of managing major gastrointestinal (GI) hemorrhage. Patients presenting with significant upper or lower GI bleeds pose unique challenges, particularly regarding airway management.
Chris offers practical advice, emphasizing the importance of resuscitating before intubation and considering video laryngoscopy in difficult cases. The post also highlights the SALAD (Suction Assisted Laryngoscopy and Airway Decontamination) technique, which is particularly useful in managing patients with large amounts of gastric contents.
Additionally, Chris touches on the use of PPIs, tranexamic acid (TXA), and terlipressin, although he advises caution until more evidence is available. The ongoing HALT-IT trial in the UK, investigating TXA in GI bleeds, is something to watch closely.
Listeriosis: A Rare but Serious Infection
Listeriosis, though uncommon, can have severe consequences, particularly for vulnerable populations like the elderly, pregnant women, newborns, and the immunocompromised. This blog post was prompted by a recent outbreak in the UK linked to contaminated hospital food.
The post emphasizes the importance of considering listeriosis in differential diagnoses, particularly for patients presenting with unexplained gastrointestinal symptoms. Blood cultures are essential for diagnosis, making it important to include them in the workup for high-risk patients. Early diagnosis is key to improving outcomes in these cases.
The Procedure Paradox: Ethical Reflections in Emergency Medicine
“The Great Day Paradox” delves into the ethical and emotional challenges of emergency medicine. Inspired by a talk at the Don’t Forget the Bubbles conference, this post explores the contrast between the excitement clinicians feel during life-saving procedures and the often devastating impact these events have on patients.
The post encourages clinicians to reflect on their motivations and maintain a patient-centered approach. Drawing on the teachings of John Hinds, it emphasizes that every procedure should be justified by both clinical need and appropriateness for the patient. This blog is a reminder of the importance of balancing clinical enthusiasm with compassion and ethical care.
Inferior Vena Cava Filters in Major Trauma: An Evidence-Based Review
Rich Carden reviewed the use of inferior vena cava (IVC) filters in major trauma patients, a topic that has been debated for years. IVC filters are intended to prevent pulmonary embolism (PE) in high-risk patients, such as those with significant lower limb or pelvic fractures.
Rich discusses a recent randomized controlled trial published in the New England Journal of Medicine, which found that early prophylactic use of IVC filters did not reduce the incidence of symptomatic pulmonary embolism or death at 90 days. This finding suggests that IVC filters should not be used routinely in major trauma patients, though there may be specific cases where they are warranted.
Psychological Performance in the Resus Room: Insights from Texas
Ashley Leibig’s presentation at St Emlyn’s Live focused on psychological performance in the resus room, drawing on her experience with StarFlight in Texas. Her blog post explores key concepts such as human factors, crew resource management, and self-awareness in high-pressure situations.
Ashley’s practical advice on managing oneself, the team, and the environment in emergency medicine is invaluable. This post is essential reading for anyone looking to improve their performance under pressure, whether in emergency medicine or other high-stress fields.
The Resuscitative Care Unit: A New Model for Emergency Departments
The concept of the resuscitative care unit (RCU) or ED-based critical care units was the focus of our final post of the month. Inspired by a paper published in the Emergency Medicine Journal (EMJ), this blog discusses the idea of creating RCUs to serve as a bridge between the emergency department and intensive care.
RCUs are proposed as a solution for managing critically ill patients who require short-term intensive care but may not need full ICU admission. The post also references a JAMA study showing that ED-based ICUs can improve survival rates for critically ill patients. As emergency departments continue to evolve, integrating critical care capabilities is becoming increasingly important.
Conclusion
July 2019 was a month filled with rich, varied content at St Emlyn’s, offering practical advice, research updates, and philosophical reflections on emergency medicine. Whether you’re interested in disaster management, GI haemorrhage, or the ethical challenges of our profession, this month’s highlights provide valuable insights.
We encourage you to engage with our content, share your thoughts, and continue learning. Don’t forget to check out our upcoming events, including the Resuscitology course and the MSc in Emergency Medicine. If you find our content valuable, please consider supporting us through a small donation to help keep St Emlyn’s free and accessible to all.
Thank you for being part of the St Emlyn’s community. We look forward to bringing you more valuable content in the coming months.

Tuesday Jul 23, 2019
Ep 142 - Psychological performance in the Resus Room with Ashley Liebig
Tuesday Jul 23, 2019
Tuesday Jul 23, 2019
This talk focuses on how we can optimise our psychological performance in critical care situations, the type of situations that Simon describes as Time Critical, Information light. The Audio is available below, or watch the full presentation above.
Don't forget to watch the video on the St Emlyn's site http://www.stemlynsblog.org
vb
S

Sunday Jul 14, 2019
Ep 141 - June 2019 Round Up
Sunday Jul 14, 2019
Sunday Jul 14, 2019
The Paradox of a Good Day in Emergency Medicine: Key Insights
Emergency medicine is a field full of paradoxes, where the definition of a "good day" can differ starkly between healthcare professionals and their patients. This contradiction was a central theme in the discussions from June, which included reflections on the Don’t Forget the Bubbles (DFTB) conference, as well as key topics like the emotional toll of emergency medicine, the evolving nature of adolescent healthcare, and the importance of continuous learning.
Don’t Forget the Bubbles Conference: A Valuable Resource for Pediatric Emergency Medicine
The DFTB conference, held in London this year, has quickly become an essential event for those involved in pediatric emergency medicine. With a focus on both pediatric and adolescent healthcare, the conference offers invaluable insights and practical advice that can benefit even those who primarily work in adult emergency medicine.
One of the standout topics from the conference was the Paradox of a Good Day in Emergency Medicine. This paradox arises from the nature of emergency medicine, where a "good day" for a clinician—filled with successful procedures and exciting cases—often coincides with what is likely the worst day of a patient’s life. This duality highlights the emotional and ethical complexities that emergency physicians must navigate. As practitioners advance in their careers, they often shift from focusing on the technical aspects of their work to becoming more aware of the profound impact these situations have on patients and their families.
The Emotional and Psychological Impact of Emergency Medicine
The emotional burden of emergency medicine was another significant theme at the DFTB conference, especially in sessions led by Kim Holt and Neil Spenceley. Holt, who has been involved in whistleblowing in the high-profile Baby P case, shared her experiences of dealing with criticism and professional challenges. Her story serves as a reminder of the resilience required to navigate the ethical and emotional complexities of healthcare.
Spenceley’s session on doctors in distress emphasized the importance of creating supportive systems within healthcare departments. He argued that instead of focusing on making individuals more resilient, we should design systems that inherently support healthcare professionals. This shift in perspective is crucial in addressing the high levels of burnout and stress among emergency medicine practitioners.
Laura Howard’s research on the psychological well-being of emergency physicians further explored this issue. Her qualitative study, which involved interviews with senior emergency physicians, revealed that the emotional impact of the job affects everyone, regardless of their experience level. Events like traumatic deaths, particularly those involving children or body disruptions, were identified as particularly distressing and had lasting effects on the practitioners involved. Howard’s work underscores the need for robust support systems to help clinicians manage the cumulative toll of their work.
Bridging the Gap in Adolescent Medicine
The DFTB conference also shed light on the often-overlooked area of adolescent healthcare. As healthcare providers, we tend to categorize patients as either adults or children, but adolescents require a tailored approach that addresses their unique needs. Russell Viner, a leader in pediatric healthcare, discussed how the concept of adolescence has evolved over time. In previous generations, adolescence was a brief period between puberty and adulthood, often marked by early milestones like starting a family. Today, however, adolescence is prolonged, with young people delaying traditional markers of adulthood due to social, educational, and economic factors.
This shift has significant implications for how we approach healthcare for adolescents. In our practice, we must ensure that we are not only addressing the physical health of teenagers but also their mental and emotional well-being. This includes creating healthcare environments that are welcoming and appropriate for adolescents and offering resources that cater to their specific health concerns.
Continuous Learning: Beyond ATLS and Traumatic Cardiac Arrest
The importance of continuous learning and staying current with the latest research and best practices was another key message from June. Alan Grayson’s talk on going beyond ATLS (Advanced Trauma Life Support) was particularly impactful. While ATLS has been a cornerstone of trauma care globally, Grayson challenged us to think critically about its limitations, especially in high-income countries where multi-disciplinary teams are the norm.
Grayson emphasized the need to focus on the basics—such as administering tranexamic acid, providing adequate analgesia, and ensuring timely administration of antibiotics—before diving into more advanced interventions like REBOA (Resuscitative Endovascular Balloon Occlusion of the Aorta). This back-to-basics approach serves as a crucial reminder that even in a high-tech medical environment, the fundamentals of care are what ultimately save lives.
Jason Smith’s session on traumatic cardiac arrest offered new insights into how we approach this challenging situation. Traditional management has focused on chest compressions, adrenaline, and fluid resuscitation, but emerging evidence suggests that in cases of traumatic cardiac arrest, these interventions may not be as beneficial as once thought. Instead, giving blood and stopping the bleeding were identified as more critical interventions. However, Smith cautioned that this approach should be reserved for hypovolemic cardiac arrest, highlighting the importance of understanding the underlying cause of the arrest before determining the treatment course.
The Reality of Intraosseous (IO) Blood Sampling
A more technical but equally important topic discussed in June was the use of intraosseous (IO) blood sampling. For years, many clinicians have been taught that IO access can provide reliable blood samples for analysis. However, recent evidence suggests otherwise. A systematic review revealed that while it might be possible to obtain certain values like hemoglobin and sodium, the reliability of these results is questionable. Moreover, using IO samples for blood gas analysis or putting marrow through automatic analyzers can lead to equipment malfunction, a concern that has understandably caused anxiety among laboratory staff.
Given this evidence, it’s clear that we need to rethink our approach to IO blood sampling. While it might still have a place in certain situations, particularly for microbiological cultures, relying on IO samples for comprehensive blood analysis is not advisable. This is another example of how continuous learning and critical evaluation of existing practices are essential for improving patient care and ensuring the best possible outcomes.
Conclusion: Moving Forward with Insights from June
As we reflect on the lessons from June, it’s evident that emergency medicine is a constantly evolving field that demands both continuous learning and emotional resilience. Whether through attending conferences like Don’t Forget the Bubbles, staying updated on the latest research, or addressing the psychological impact of our work, it’s clear that adaptation and mutual support are key to thriving in this challenging yet rewarding profession.
At St Emlyn's, we are committed to fostering a culture of lifelong learning, open discussion, and mutual support. As we move into the second half of the year, let’s carry forward the insights we’ve gained, keep pushing the boundaries of our knowledge, and continue to support each other in the demanding yet rewarding field of emergency medicine. Take care, and keep up the incredible work you do.

Thursday Jul 04, 2019
Ep 140 - GI emergencies with Chris Gray at #stemlynsLIVE
Thursday Jul 04, 2019
Thursday Jul 04, 2019
This is Chris's talk from #stemlynsLIVE on GI emergencies. Remember to check out the blog for the background, references and more.

Friday Jun 21, 2019
Ep 139 - May 2019 Round Up
Friday Jun 21, 2019
Friday Jun 21, 2019
St. Emlyn's Podcast: Key Insights from May in Emergency Medicine
As we transition into the warmer months, it's an opportune time to reflect on recent discussions and developments within the field of emergency medicine, particularly those highlighted in the latest episode of the St. Emlyn's podcast. This episode covered a wide range of topics, from workplace safety to advancements in pediatric care and innovative approaches in patient management. Below is a comprehensive summary of the key points discussed.
Workplace Safety: A Pressing Concern
The podcast began with a reflection on a recent violent incident at Newham Emergency Department (ED), which served as a stark reminder of the dangers healthcare professionals face daily. Emergency departments, by their very nature, are open and accessible, making them vulnerable to violent incidents. This recent attack has prompted a nationwide reassessment of safety measures, with many EDs enhancing their protocols to protect staff.
The conversation emphasized that violence in the workplace should never be normalized. It’s crucial that healthcare professionals feel safe and supported in their working environment. Leadership within departments plays a critical role in this, not only by implementing robust safety protocols but also by fostering a culture of solidarity and mutual support among staff. The incident at Newham underscores the need for constant vigilance and proactive measures to ensure the safety of everyone working in emergency medicine.
Leadership in Education: Simon Carley’s New Role
In more positive news, Simon Carley’s recent appointment as the CPD (Continuing Professional Development) lead for the college was discussed. This role is a significant milestone, not just for Simon but also for the integration of modern educational approaches within formal medical education. Simon’s involvement with St. Emlyn's has long been focused on innovative, social media-driven education, and this new role offers an opportunity to bring these methods into a broader educational framework.
The appointment highlights the value of combining traditional education with the dynamic, accessible formats offered by the #FOAMed (Free Open Access Meducation) community. It’s a recognition that medical education can benefit from new perspectives and that the integration of these ideas can enhance the learning experiences for healthcare professionals.
Pediatric Status Epilepticus: Evaluating Second-Line Agents
The discussion moved to a detailed analysis of pediatric status epilepticus, focusing on the findings from two key trials: the Eclipse trial and the ConSEPT trial. These studies compared the efficacy of levetiracetam (Keppra) and phenytoin as second-line agents for stopping seizures in children.
The trials found no significant difference between the two drugs in terms of their effectiveness, which has led to debate within the medical community about whether to switch from phenytoin to levetiracetam. While levetiracetam is perceived as easier to administer and safer, the lack of a clear superiority has left the decision somewhat open. However, the ease of use and safety profile of levetiracetam make it an appealing option, and some institutions are considering making the switch.
For clinicians, the takeaway is that while both drugs are viable options, the choice may ultimately come down to individual preferences and institutional protocols. The trials underscore the importance of continuous evaluation of treatment options, particularly in complex cases like pediatric seizures.
Understanding Clinical Trials: The Importance of Statistical Literacy
Simon Carley also highlighted the importance of understanding the statistical nuances in clinical trials, particularly the difference between demonstrating a difference between treatments and establishing their equivalence. This distinction is crucial for accurately interpreting research findings and making informed clinical decisions.
The discussion emphasized that clinicians must be cautious in how they interpret trial results, particularly when it comes to determining whether treatments are genuinely equivalent or if the lack of a significant difference merely reflects the study’s design. This level of critical appraisal is essential for ensuring that new research is applied correctly in clinical practice.
Prolonged Field Care in the ED: Learning from Military Medicine
Another topic discussed was prolonged field care, a concept borrowed from military medicine that is becoming increasingly relevant in emergency departments due to overcrowding and delays. Rich Carden introduced the HITMAN mnemonic—Hygiene and Hydration, Infection, Tubes, Medication, Analgesia, and Nutrition—as a framework for managing patients who are stuck in the ED for extended periods.
The HITMAN approach ensures that patients' fundamental needs are met even when resources are stretched. This method helps prevent complications and improves patient outcomes, even in less-than-ideal conditions. The approach is particularly relevant in today’s healthcare environment, where EDs are often overwhelmed and patients may wait longer than usual for admission or transfer.
Atrial Fibrillation: Reassessing Cardioversion Strategies
Atrial fibrillation (AF) management was another key topic. A recent study in the New England Journal of Medicine compared immediate cardioversion with a wait-and-see approach in patients with new-onset AF. The study found that a wait-and-see approach was non-inferior to immediate cardioversion, with 69% of patients in the wait-and-see group spontaneously cardioverting within 48 hours.
This finding challenges the traditional approach of immediate cardioversion and suggests that in many cases, a more conservative approach may be just as effective. However, the decision should be made through shared decision-making with the patient, taking into account their preferences and the specific circumstances of their condition. This patient-centered approach ensures that treatment decisions are made collaboratively and with the patient’s best interests in mind.
Traumatic Cardiac Arrest: Reevaluating Chest Compressions
The podcast also touched on the evolving management of traumatic cardiac arrest, particularly the role of chest compressions. Recent studies, including one involving porcine models, suggest that in cases of hypovolemic traumatic cardiac arrest, chest compressions may not be beneficial and could even be harmful. Instead, the focus should be on addressing the underlying cause, such as restoring circulating volume.
This shift in practice highlights the importance of understanding the specific etiology of cardiac arrest and tailoring resuscitation efforts accordingly. Communicating these changes to the entire resuscitation team is crucial, as there may be resistance to deviating from traditional protocols. Ensuring that everyone is on the same page and understands the rationale behind the approach is key to successful implementation.
Virtual Reality in Pain Management: An Emerging Tool
Virtual reality (VR) is emerging as a promising tool in pain management, particularly in pediatric patients undergoing painful procedures. A recent study discussed in the podcast found that children who used VR experienced less distress during procedures compared to those who received standard care.
VR offers an innovative, accessible method for managing pain and anxiety, and its use is likely to expand in the coming years. The ability to create immersive environments that distract patients during procedures has the potential to improve patient experiences and outcomes, not just in children but potentially in adults as well.
The Power of Peer Review: Enhancing Clinical Practice
Finally, Simon Carley discussed the importance of peer review in clinical practice. Peer review is a valuable tool for continuous improvement, allowing clinicians to receive feedback from colleagues on their performance. While it can be challenging to create a culture where feedback is welcomed and constructive, the benefits are significant.
Peer review helps clinicians avoid complacency, stay up-to-date with best practices, and continually refine their skills. It’s a simple, cost-effective way to ensure that healthcare professionals are delivering the highest standard of care. Creating a supportive environment where feedback is seen as an opportunity for growth rather than criticism is essential for the success of peer review initiatives.
Conclusion
The discussions in this month’s St. Emlyn's podcast highlight the complexities and challenges of working in emergency medicine, from ensuring workplace safety to staying current with evolving practices. By engaging with new research, embracing innovative tools like virtual reality, and fostering a culture of continuous improvement through peer review, we can continue to advance the field and improve patient care. As always, the St. Emlyn's blog and podcast remain valuable resources for staying informed and connected with the latest developments in emergency medicine.

Wednesday Apr 24, 2019
Ep 134 - March 2019 Round Up
Wednesday Apr 24, 2019
Wednesday Apr 24, 2019
Highlights from March 2019: Key Insights and Updates
Welcome to the St Emlyn's podcast. I'm Simon Carley and today; I'll be taking you through the highlights from our blog in March 2019. This was a busy month filled with exceptional content, insightful trips, and significant conferences. Let's dive into the details and explore some key topics, starting with adult congenital heart disease, top trauma papers, and the importance of responsible volunteering.
Management of Adult Congenital Heart Disease
March kicked off with an important post on the management of adult congenital heart disease (ACHD). This topic is particularly close to my heart as the hospital I work at is a level two centre for ACHD in the UK. Services have become centralized, and surgical components are now managed at a few specialized centres, with Liverpool being the hub for my region.
Despite this centralization, we still encounter a large population of ACHD patients in our area. These patients often present complex medical histories and unique pathologies that can be challenging to manage in emergency settings. The guidance available typically focuses on chronic and surgical management, but emergency care for these patients requires a different approach.
Common Issues in ACHD Patients
ACHD patients commonly present with dysrhythmias, which can be particularly challenging to manage. Chest pain is also prevalent, although the incidence of ischemic heart disease isn’t significantly higher in ACHD patients, except for those who have undergone certain procedures like the switch operation. Other common issues include:
- Cyanotic patients: Those with single ventricle physiology and right-to-left shunts.
- Endocarditis: A rare but serious complication.
- Non-cardiac problems: Managing ACHD patients with conditions like appendicitis or pneumonia can be complex due to their unique circulatory dynamics.
The bottom line is that these patients often require specialized management strategies. When ACHD patients present with cardiac complications, we consult our local cardiologist or the ACHD centre. However, non-cardiac issues in ACHD patients also warrant discussion with the ACHD centre to ensure comprehensive care.
Key Takeaways for Emergency Physicians
Emergency physicians should familiarize themselves with the unique aspects of Fontan circulation, which relies on venous return based on venous pressure. Aggressive interventions like CPAP, bagging, and diuretics can be detrimental. Understanding these nuances is crucial for providing optimal care.
A Deeper Dive into Fontan Circulation
The Fontan procedure, a surgical intervention for single ventricle defects, creates a unique circulatory system that can be difficult to manage in emergency settings. Unlike normal circulation, Fontan physiology depends heavily on passive blood flow from the veins to the lungs. This means that increasing intrathoracic pressure through methods like CPAP or bagging can reduce cardiac output and worsen the patient's condition.
Fontan patients are particularly vulnerable to fluid shifts and pressures, making careful management of intravenous fluids and medications essential. Understanding these dynamics can be life-saving in the ED. For example, while diuretics might seem a reasonable choice for a patient with fluid overload, they can lead to dangerously low preload and cardiac output in a Fontan patient.
Top Trauma Papers from the Trauma UK Conference
Next up, we revisited some of the top trauma papers presented at the Trauma UK conference. These papers covered a range of topics, from the use of bougies in the ED to bag-mask ventilation during hypertensive resuscitation. Here are some key highlights:
The PAMPer Trial
The PAMPer trial examined the use of prehospital plasma in trauma patients and found significant survival benefits. This trial has important implications for trauma care protocols, emphasizing the potential of early plasma administration to improve outcomes.
The trial showed that administering plasma before hospital arrival can reduce mortality rates in severely injured patients. This finding supports the concept of damage control resuscitation, aiming to stabilize patients early and prevent coagulopathy, acidosis, and hypothermia—the lethal triad in trauma.
Bougie Use in the ED
Another focal point was the utility of bougies in emergency airway management. Evidence suggests that bougies can significantly improve first-pass success rates in difficult intubations, making them a valuable tool in the ED.
A study highlighted at the conference demonstrated that the use of a bougie, even in routine intubations, could increase the success rates for first-pass intubations. This is particularly important in prehospital settings and emergency departments where difficult airways are common.
Late Presenting Head Injury Patients
A paper from Hull explored the management of patients presenting with head injuries more than 24 hours post-injury. The findings indicated that these patients have a significant incidence of important findings on CT scans, suggesting that delayed presentations should not be underestimated.
This study challenges the conventional exclusion of late-presenting head injury patients from acute imaging protocols. It suggests that significant injuries can still be present and warrant immediate attention, even if the patient presents days after the initial trauma.
The Zero Point Survey
The Zero Point Survey, which emphasizes situational awareness, team dynamics, and environmental control before initiating the primary survey, was also highlighted. This approach can significantly enhance resuscitation efforts, ensuring a more organized and effective response.
The Zero Point Survey encourages clinicians to prepare mentally and physically before patient contact. By assessing the situation, assembling the right team, and ensuring the environment is conducive to optimal care, clinicians can improve outcomes and reduce errors in high-stress scenarios.
Responsible Volunteering Overseas
One of the most thought-provoking posts of the month came from Stefan Brisions, discussing the need for responsible volunteering overseas. Volunteering in low and middle-income countries can be incredibly rewarding, but it’s essential to approach it with the right mindset and framework.
The Ethics of Volunteering
Stefan emphasized the importance of volunteering within a system that has sustainability and benefits for all parties involved. There have been concerns about individuals volunteering for personal gain rather than genuine altruism. It’s crucial to ensure that our efforts are focused on creating lasting, positive impacts.
Volunteering should always aim to build local capacity rather than create dependency. This means working with local healthcare providers to enhance their skills and infrastructure, ensuring that the benefits of volunteering continue long after volunteers have left.
Volunteering Responsibly
If you're considering volunteering abroad, it’s vital to engage with established organizations that have a clear mission and ethical framework. This ensures that your contributions are meaningful and aligned with the needs of the local community. Our discussions with experts like Shweta Gidwani, Hooling Harrison, Jennifer Hulls, and Najee Rahman offer valuable insights into this complex issue.
Case Study: Volunteering in South Africa
Kat Evans, who works in Mitchell’s Plain in South Africa, shared her experiences at St Emlyn’s Live. Kat discussed the challenges of working in a resource-limited environment, particularly in managing trauma and toxicology cases.
Her insights into managing trauma in a high-volume, low-resource setting were eye-opening. Kat also shared fascinating details about the use of high doses of atropine for poisoning cases, highlighting the unique medical practices required in such environments.
Kat’s presentation underscored the value of structured volunteer programs that integrate volunteers into local healthcare systems, providing both valuable learning experiences and much-needed support to local healthcare providers.
The Future of SMACC: CODA
March also marked the end of an era with the final SMACC conference in Sydney. SMACC has been a cornerstone for many in the emergency and critical care communities, offering unparalleled opportunities for learning and networking. However, the spirit of SMACC lives on in its successor, CODA.
CODA: A New Beginning
CODA aims to build on SMACC's successes while addressing broader health issues such as vaccination, climate change, and healthcare inequality. The goal is to leverage the engaged community SMACC created to drive meaningful change on a global scale.
CODA plans to tackle these global health issues by bringing together a diverse group of professionals, including those outside the traditional medical fields. This interdisciplinary approach aims to create innovative solutions to some of the world’s most pressing health challenges.
Looking Ahead
While we bid farewell to SMACC, we look forward to the new opportunities CODA will bring. Its emphasis on tackling significant health challenges aligns with the evolving needs of the global healthcare community, promising an exciting future.
What to Expect from CODA
CODA will continue the tradition of high-quality content and dynamic presentations that SMACC was known for. However, it will also incorporate new elements focused on global health advocacy and interdisciplinary collaboration. Expect to see more discussions on how healthcare professionals can contribute to solving broader societal issues.
Additional Highlights from March
Critical Appraisal Nuggets (CANS) on P-values
We also introduced a mini podcast series called Critical Appraisal Nuggets (CANS) focusing on p-values, featuring myself and Rick Body. P-values are a common topic in exams and critical appraisal, and understanding them is crucial for interpreting medical research.
This less-than-ten-minute podcast provides a concise overview of p-values, helping clinicians and students alike grasp this important concept. By demystifying p-values, we aim to enhance our audience's critical appraisal skills, enabling better evidence-based practice.
Dual Coding in Medical Education
Nick Smith, a recent addition to the St Emlyn's team and a brilliant clinical educator, shared insights on dual coding. Dual coding involves using both verbal and visual information to enhance learning and retention.
Nick’s post emphasized how our brains struggle to process multiple streams of information simultaneously. Effective teaching and communication require a balance between verbal explanations and visual aids, ensuring that learners can absorb and retain information without being overwhelmed.
The Impact of Reboa in Trauma Care
Zaf Qasim, a great friend of ours over in the US, examined the impact of Resuscitative Endovascular Balloon Occlusion of the Aorta (Reboa) in trauma care. This post, based on a paper published in JAMA Surgery, analyzed Reboa success rates in civilian trauma using a US database.
The findings suggested that Reboa was associated with higher mortality rates compared to similar patients who did not receive Reboa. This raises important questions about patient selection and the overall benefits of Reboa in trauma care.
Zaf’s post highlighted the need for ongoing research and evidence to determine Reboa's true value. While there are compelling pathophysiological arguments for its use, the clinical outcomes must be scrutinized to ensure it is applied appropriately and effectively.
The Role of Evidence-Based Practice
At St Emlyn's, we prioritize evidence-based practice in all aspects of emergency medicine. The discussions around Reboa, p-values, and dual coding all reinforce the importance of using high-quality evidence to guide clinical decisions and educational strategies.
Final Thoughts
March 2019 was a month of incredible learning and growth. From managing complex ACHD patients to discussing the ethics of volunteering and exploring cutting-edge trauma research, we covered a wide range of topics that are crucial for emergency medicine professionals.
Stay Connected
As we move forward, we encourage you to stay connected with St Emlyn’s for more insights, updates, and discussions. Follow our blog, participate in our events, and join the conversation on social media. Together, we can continue to advance the field of emergency medicine and make a difference in the lives of our patients.
Thank you for joining us this month. Enjoy your practice, and we’ll be back with more great content in April. Have fun, stay safe, and keep learning!

Saturday Apr 13, 2019
Ep 133 - February 2019 Round Up
Saturday Apr 13, 2019
Saturday Apr 13, 2019
Exploring the Latest in Emergency Medicine: February 2024 Edition
Hello and welcome to the St Emlyn's Podcast! I’m Simon Carly, and today, albeit a little later than planned, I'll be diving into the fascinating February papers and blogs that have graced the St Emlyn's Podcast. If you missed out in February, fear not—you can always revisit the archives on our blog. It’s all there, waiting for you to explore. Let’s take a deep dive into what made February such an exciting month in emergency medicine.
A Journey to Jeddah: Bridging Borders in Emergency Medicine
In February, I had the distinct honour of travelling to Jeddah, Saudi Arabia, to join the Saudi Arabian Society of Emergency Medicine. Jeddah is a city brimming with activity and change. Despite Saudi Arabia being vastly different from the UK, I found common ground with the emergency physicians there. Many of them have trained abroad in Canada, the US, and the UK, making them kindred spirits with shared values and ideas in treating emergency patients.
During my visit, I was invited to present the top ten trauma papers, a task I thoroughly enjoy. These papers, detailed on our website, included highlights like the PAMPER trial and airway management papers around cardiac arrest. We also delved into studies beyond trauma, such as the Airways 2 study on superox in critically ill patients and intubation with ED use of bougies, which we advocate at St. Emlyn’s. Additionally, the conservative management of pneumothoraces, a topic we've discussed before, is becoming increasingly recognized as safe, especially for traumatic pneumothoraces visible only on CT scans.
PTSD and the Road to Recovery: Insights from Rusty Carroll
Our friend and colleague, Rusty Carroll, has shared another compelling post on PTSD. Rusty’s previous blogs detailed his recovery journey from PTSD, stemming from his work in the ambulance service. His latest update brings us into his post-therapy life as he navigates a new, rewarding, and successful path. For anyone experiencing PTSD or knowing someone who is, Rusty's series is invaluable. His journey may differ from yours, but understanding that there is a path to recovery is incredibly encouraging.
PTSD is a serious issue that affects many healthcare professionals, and Rusty’s openness about his struggles and recovery provides a beacon of hope for others. His posts cover various aspects of his journey, from the initial recognition of symptoms to the therapeutic interventions that helped him reclaim his life. Rusty emphasizes the importance of seeking help, breaking the stigma associated with mental health issues, and supporting colleagues who may be going through similar experiences.
Understanding Trauma Mortality: A Shift in Focus
In our journal club, we explored why bleeding trauma patients die. This editorial by Karen Broe and John Holcomb in Critical Care Medicine challenges our preconceptions about trauma mortality. The implementation of pre-hospital systems, emergency management, and damage control surgery has significantly reduced pre-hospital deaths. However, this has shifted mortality to the emergency department's early hours and even later, 24 hours down the line.
We are now seeing deaths caused by late systematic immunosuppression, persistent inflammation, and catabolism syndromes. Despite successful initial management, patients are still succumbing later on. This shift indicates that our trauma story is far from complete. More research is needed to understand and address these late-phase deaths, suggesting that critical care phases hold the key to future advancements.
This new understanding prompts us to reconsider our approaches in trauma care. While we have made significant strides in reducing early mortality, the challenge now lies in managing these complex late-phase issues. This involves multidisciplinary collaboration, innovative research, and a commitment to continuous improvement in trauma care protocols.
Reevaluating PE in Syncope: A Fresh Perspective
Natalie May published a follow-up paper related to the PESIT study, which had previously suggested a high incidence of pulmonary embolism (PE) as a cause of syncope. This controversial study, conducted in Italy, sparked debates across various platforms, including EM Nerd, EMCrit, Emlyns Note, and Rebel EM.
However, new research from the North American Syncope Consortium reveals a much lower prevalence of PE among emergency department patients with syncope. This is a significant finding, as it challenges the alarming figures from the PESIT study. It allows us to return to our previous practices of using well-established tools like Wells' scoring and PERC scoring without the heightened fear of PE being the primary cause of syncope.
Natalie’s analysis provides a balanced perspective, highlighting the importance of context in interpreting study results. The discrepancy between the PESIT study and the North American Syncope Consortium's findings underscores the need for ongoing research and validation of clinical guidelines. As emergency physicians, staying informed about such developments ensures that we provide the best care based on the latest evidence.
Philosophy of Emergency Medicine: Workplace Relationships Matter
Stefan Brzezins contributes a thought-provoking post on the importance of workplace relationships. Stefan, a colleague who has worked in South Africa and now the UK, highlights how our interactions with colleagues significantly impact our behaviour, happiness, and departmental efficiency. Dysfunctional departments often correlate with poor personal relationships among consultants and senior nurses, ultimately affecting patient care.
Stefan's advice includes not taking unnecessary offence, showing gratitude, celebrating the good news, and fostering teamwork. While these may seem obvious, their implementation can transform workplace dynamics. Reflecting on Stefan's insights has prompted me to reevaluate my practices and strive for better interpersonal relationships at work.
Good workplace relationships are foundational to creating a supportive and effective healthcare environment. When colleagues communicate openly, show appreciation for each other’s efforts, and work collaboratively, they experience higher job satisfaction, reduced stress, and, ultimately, better patient outcomes. Stefan’s post serves as a reminder that the human element of healthcare is just as important as the clinical skills we bring to our practice.
Ventilation During RSI: Revisiting Established Practices
Another significant post examines whether we should continue ventilation during rapid sequence intubation (RSI). Traditional teaching discouraged ventilation during the apnea period due to safety concerns. However, for critically ill patients with low oxygen saturation, not ventilating can lead to severe hypoxia.
A randomized control trial in the ED assessed the safety of ventilation during this period. The study found that patients who were ventilated during the apnea period had less oxygen desaturation without significant adverse effects. While the study's sample size is small, it supports our evolving practices and aligns with our experiences. However, it is crucial to critically assess the study's methodology and incorporate this knowledge cautiously into clinical practice.
This trial’s findings challenge the long-standing dogma of no ventilation during RSI, pushing us to rethink and potentially update our protocols. As emergency medicine evolves, we must remain flexible and willing to adapt our practices based on emerging evidence. Ensuring that our approaches are both safe and effective is paramount to improving patient outcomes.
The Role of Scribes in the ED: Efficiency and Quality Improvement
Chris Gray's post on the use of scribes in the ED follows a previous discussion on this topic. Scribes can save time and improve documentation quality, which is vital in a high-pressure environment. A randomized control trial demonstrated that scribes do save time, though the effect size was modest. The potential for better documentation quality is equally important, making scribes a valuable addition to emergency departments. We are keen to hear from anyone using scribes in the UK, as this practice is more common in the US.
The use of scribes can enhance the efficiency of emergency departments by allowing physicians to focus more on patient care rather than administrative tasks. Improved documentation can also lead to better patient tracking, follow-up, and overall care quality. As our healthcare systems become increasingly strained, innovations like scribes offer practical solutions to maintain high standards of care.
Reflecting on February: A Busy Month in Emergency Medicine
February was packed with insights and developments in emergency medicine. From international collaborations and trauma management advancements to revisiting PTSD recovery stories and philosophical reflections on workplace relationships, the month offered a wealth of knowledge. As we move into March, we look forward to sharing more exciting updates, including coverage of the SMACC conference.
The diversity of topics covered in February highlights the multifaceted nature of emergency medicine. Each paper and blog post contributes to a broader understanding of how we can improve patient care, support our colleagues, and adapt to new challenges. This continuous learning process is what makes emergency medicine such a dynamic and rewarding field.
Supporting the St Emlyn's Podcast: Your Contribution Matters
Since 2012, we've funded the blog and podcast out of our own pockets. As our audience grows, so do our expenses. If you find our content valuable and wish to support us, please consider making a small donation or subscribing regularly. Your contributions help us keep St Emlyn's a free, open-access medical education resource for all.
By supporting the St Emlyn's Podcast, you enable us to continue delivering high-quality, evidence-based content to the emergency medicine community. Your donations help cover the costs of hosting, producing, and distributing our materials, ensuring that we can reach a global audience of healthcare professionals.
Conclusion
The February edition of the St Emlyn's Podcast provided a rich tapestry of insights and developments in emergency medicine. From my journey to Jeddah and the fascinating trauma studies to the personal stories of PTSD recovery and the philosophical reflections on workplace relationships, there was something for everyone.
Our exploration of new research, such as the reevaluation of PE in syncope and the safety of ventilation during RSI, underscores the importance of staying informed and adaptable in our practice. Meanwhile, discussions on the role of scribes and the significance of workplace dynamics highlight the multifaceted challenges we face in emergency medicine.
As we look forward to March and beyond, we remain committed to bringing you the latest in emergency medicine and fostering a community of continuous learning and improvement. Thank you for joining us on this journey, and we appreciate your support in keeping St Emlyn's a vital resource for all.
Stay tuned for more insights, updates, and discussions. Until then, keep pushing the boundaries of emergency medicine, supporting your colleagues, and striving for excellence in patient care. Have a great time, and we’ll be back with you shortly.
Exploring the Latest in Emergency Medicine: February 2024 Edition
Hello and welcome to the St Emlyn's Podcast! I’m Simon Carly, and today, albeit a little later than planned, I'll be diving into the fascinating February papers and blogs that have graced the St Emlyn's Podcast. If you missed out in February, fear not—you can always revisit the archives on our blog. It’s all there, waiting for you to explore. Let’s take a deep dive into what made February such an exciting month in emergency medicine.
A Journey to Jeddah: Bridging Borders in Emergency Medicine
In February, I had the distinct honour of travelling to Jeddah, Saudi Arabia, to join the Saudi Arabian Society of Emergency Medicine. Jeddah is a city brimming with activity and change. Despite Saudi Arabia being vastly different from the UK, I found common ground with the emergency physicians there. Many of them have trained abroad in Canada, the US, and the UK, making them kindred spirits with shared values and ideas in treating emergency patients.
During my visit, I was invited to present the top ten trauma papers, a task I thoroughly enjoy. These papers, detailed on our website, included highlights like the PAMPER trial and airway management papers around cardiac arrest. We also delved into studies beyond trauma, such as the Airways 2 study on superox in critically ill patients and intubation with ED use of bougies, which we advocate at St. Emlyn’s. Additionally, the conservative management of pneumothoraces, a topic we've discussed before, is becoming increasingly recognized as safe, especially for traumatic pneumothoraces visible only on CT scans.
PTSD and the Road to Recovery: Insights from Rusty Carroll
Our friend and colleague, Rusty Carroll, has shared another compelling post on PTSD. Rusty’s previous blogs detailed his recovery journey from PTSD, stemming from his work in the ambulance service. His latest update brings us into his post-therapy life as he navigates a new, rewarding, and successful path. For anyone experiencing PTSD or knowing someone who is, Rusty's series is invaluable. His journey may differ from yours, but understanding that there is a path to recovery is incredibly encouraging.
PTSD is a serious issue that affects many healthcare professionals, and Rusty’s openness about his struggles and recovery provides a beacon of hope for others. His posts cover various aspects of his journey, from the initial recognition of symptoms to the therapeutic interventions that helped him reclaim his life. Rusty emphasizes the importance of seeking help, breaking the stigma associated with mental health issues, and supporting colleagues who may be going through similar experiences.
Understanding Trauma Mortality: A Shift in Focus
In our journal club, we explored why bleeding trauma patients die. This editorial by Karen Broe and John Holcomb in Critical Care Medicine challenges our preconceptions about trauma mortality. The implementation of pre-hospital systems, emergency management, and damage control surgery has significantly reduced pre-hospital deaths. However, this has shifted mortality to the emergency department's early hours and even later, 24 hours down the line.
We are now seeing deaths caused by late systematic immunosuppression, persistent inflammation, and catabolism syndromes. Despite successful initial management, patients are still succumbing later on. This shift indicates that our trauma story is far from complete. More research is needed to understand and address these late-phase deaths, suggesting that critical care phases hold the key to future advancements.
This new understanding prompts us to reconsider our approaches in trauma care. While we have made significant strides in reducing early mortality, the challenge now lies in managing these complex late-phase issues. This involves multidisciplinary collaboration, innovative research, and a commitment to continuous improvement in trauma care protocols.
Reevaluating PE in Syncope: A Fresh Perspective
Natalie May published a follow-up paper related to the PESIT study, which had previously suggested a high incidence of pulmonary embolism (PE) as a cause of syncope. This controversial study, conducted in Italy, sparked debates across various platforms, including EM Nerd, EMCrit, Emlyns Note, and Rebel EM.
However, new research from the North American Syncope Consortium reveals a much lower prevalence of PE among emergency department patients with syncope. This is a significant finding, as it challenges the alarming figures from the PESIT study. It allows us to return to our previous practices of using well-established tools like Wells' scoring and PERC scoring without the heightened fear of PE being the primary cause of syncope.
Natalie’s analysis provides a balanced perspective, highlighting the importance of context in interpreting study results. The discrepancy between the PESIT study and the North American Syncope Consortium's findings underscores the need for ongoing research and validation of clinical guidelines. As emergency physicians, staying informed about such developments ensures that we provide the best care based on the latest evidence.
Philosophy of Emergency Medicine: Workplace Relationships Matter
Stefan Brzezins contributes a thought-provoking post on the importance of workplace relationships. Stefan, a colleague who has worked in South Africa and now the UK, highlights how our interactions with colleagues significantly impact our behaviour, happiness, and departmental efficiency. Dysfunctional departments often correlate with poor personal relationships among consultants and senior nurses, ultimately affecting patient care.
Stefan's advice includes not taking unnecessary offence, showing gratitude, celebrating the good news, and fostering teamwork. While these may seem obvious, their implementation can transform workplace dynamics. Reflecting on Stefan's insights has prompted me to reevaluate my practices and strive for better interpersonal relationships at work.
Good workplace relationships are foundational to creating a supportive and effective healthcare environment. When colleagues communicate openly, show appreciation for each other’s efforts, and work collaboratively, it leads to higher job satisfaction, reduced stress, and ultimately better patient outcomes. Stefan’s post serves as a reminder that the human element of healthcare is just as important as the clinical skills we bring to our practice.
Ventilation During RSI: Revisiting Established Practices
Another significant post examines whether we should continue ventilation during rapid sequence intubation (RSI). Traditional teaching discouraged ventilation during the apnea period due to safety concerns. However, for critically ill patients with low oxygen saturation, not ventilating can lead to severe hypoxia.
A randomized control trial in the ED assessed the safety of ventilation during this period. The study found that patients who were ventilated during the apnea period had less oxygen desaturation without significant adverse effects. While the study's sample size is small, it supports our evolving practices and aligns with our experiences. However, it is crucial to critically assess the study's methodology and incorporate this knowledge cautiously into clinical practice.
This trial’s findings challenge the long-standing dogma of no ventilation during RSI, pushing us to rethink and potentially update our protocols. As emergency medicine evolves, we must remain flexible and willing to adapt our practices based on emerging evidence. Ensuring that our approaches are both safe and effective is paramount to improving patient outcomes.
The Role of Scribes in the ED: Efficiency and Quality Improvement
Chris Gray's post on the use of scribes in the ED follows a previous discussion on this topic. Scribes can save time and improve documentation quality, which is vital in a high-pressure environment. A randomized control trial demonstrated that scribes do save time, though the effect size was modest. The potential for better documentation quality is equally important, making scribes a valuable addition to emergency departments. We are keen to hear from anyone using scribes in the UK, as this practice is more common in the US.
The use of scribes can enhance the efficiency of emergency departments by allowing physicians to focus more on patient care rather than administrative tasks. Improved documentation can also lead to better patient tracking, follow-up, and overall care quality. As our healthcare systems become increasingly strained, innovations like scribes offer practical solutions to maintain high standards of care.
Reflecting on February: A Busy Month in Emergency Medicine
February was packed with insights and developments in emergency medicine. From international collaborations and trauma management advancements to revisiting PTSD recovery stories and philosophical reflections on workplace relationships, the month offered a wealth of knowledge. As we move into March, we look forward to sharing more exciting updates, including coverage of the SMACC conference.
The diversity of topics covered in February highlights the multifaceted nature of emergency medicine. Each paper and blog post contributes to a broader understanding of how we can improve patient care, support our colleagues, and adapt to new challenges. This continuous learning process is what makes emergency medicine such a dynamic and rewarding field.
Supporting the St Emlyn's Podcast: Your Contribution Matters
Since 2012, we've funded the blog and podcast out of our own pockets. As our audience grows, so do our expenses. If you find our content valuable and wish to support us, please consider making a small donation or subscribing regularly. Your contributions help us keep St Emlyn's a free, open-access medical education resource for all.
By supporting the St Emlyn's Podcast, you enable us to continue delivering high-quality, evidence-based content to the emergency medicine community. Your donations help cover the costs of hosting, producing, and distributing our materials, ensuring that we can reach a global audience of healthcare professionals.
Conclusion
The February edition of the St Emlyn's Podcast provided a rich tapestry of insights and developments in emergency medicine. From my journey to Jeddah and the fascinating trauma studies to the personal stories of PTSD recovery and the philosophical reflections on workplace relationships, there was something for everyone.
Our exploration of new research, such as the reevaluation of PE in syncope and the safety of ventilation during RSI, underscores the importance of staying informed and adaptable in our practice. Meanwhile, discussions on the role of scribes and the significance of workplace dynamics highlight the multifaceted challenges we face in emergency medicine.
As we look forward to March and beyond, we remain committed to bringing you the latest in emergency medicine and fostering a community of continuous learning and improvement. Thank you for joining us on this journey, and we appreciate your support in keeping St Emlyn's a vital resource for all.
Stay tuned for more insights, updates, and discussions. Until then, keep pushing the boundaries of emergency medicine, supporting your colleagues, and striving for excellence in patient care. Have a great time, and we’ll be back with you shortly.

Friday Mar 15, 2019
Ep 131 - South African Emergency Medicine with Kat Evans at #stemlynsLIVE
Friday Mar 15, 2019
Friday Mar 15, 2019
Last year we were honoured to bring Kat Evans to Manchester to talk at the #stemlynsLIVE conference. We've covered emergency medicine in South Africa before on the blog, but there is no substitute to hearing about it from someone who actually works there.

Sunday Feb 17, 2019
Ep 129 - January 2019 Round Up
Sunday Feb 17, 2019
Sunday Feb 17, 2019
St. Emlyn's January Roundup: Key Insights and Innovations
Hello and welcome to the St. Emlyn’s Podcast. I’m Simon Carley, joined by Rick Body. Today, we’re bringing you our January roundup, sharing the most intriguing and impactful content we've covered this month. From reflecting on 2018 to exploring new guidelines and innovations in emergency medicine, we have a lot to discuss. Let’s dive in!
Reflecting on 2018: Transformational Reads and Achievements
As we started January, we reflected on 2018, a year filled with significant achievements and insights. One standout discussion was our review of key books that left a lasting impact. A personal favorite of mine is "Why We Sleep" by Matthew Walker. This book has been transformational for me, influencing how I live and advise others on health, well-being, and performance. The insights on sleep’s importance in education, creativity, and overall health are profound.
Rick, did anything from our 2018 review resonate with you?
Rick Body: Absolutely, Simon. The variety of books we discussed was impressive. It was enlightening to hear about others' achievements in 2018 and their goals for 2019. This exercise really focused my mind on what I hope to achieve this year.
Goals for 2019: Innovations and Personal Aspirations
As we moved from reflections to aspirations, we set our sights on exciting projects for 2019. One major highlight is the AI incubator for emergency care. This initiative aims to support academic careers and foster partnerships between data and industry to enhance medical technologies. It’s an exhilarating time for advancements in emergency care.
Rick is incredibly busy with groundbreaking work, particularly in diagnostics in Manchester. His research and speaking engagements are making waves in the medical community. For more details on these projects, check out the blog where all the information is comprehensively covered.
New Year’s Resolutions: Insights from Liz Crowe
We explored New Year’s resolutions with Liz Crowe, who offered a fresh perspective on well-being and resolutions. Instead of focusing on all-or-nothing goals, Liz suggests starting small and seeking rewards rather than punishments. This approach makes significant lifestyle changes more manageable and sustainable. Committing to resolutions publicly or with a friend can enhance accountability and success.
Rick, do you have any New Year’s resolutions?
Rick Body: It’s challenging to pinpoint one or two, but Liz’s advice on avoiding binary thinking is crucial. Recognizing progress rather than dwelling on setbacks can make a big difference.
Tetanus Guidelines: New Insights and Practical Applications
In January, we delved into updated tetanus guidelines, highlighting significant changes. Previously, a single booster in your early 20s was deemed sufficient, but the new guidelines recommend a 10-year booster. This change stems from the recognition that immunity wanes over time. Interestingly, point-of-care testing is now available to detect active tetanus immunization, allowing for more tailored booster decisions.
These updates are crucial for emergency physicians to ensure compliance with current standards and provide optimal patient care. The blog post simplifies these guidelines, making them accessible and easy to understand.
Excellence in Emergency Medicine: Claire Richmond’s Contributions
We featured Claire Richmond, a hero in the emergency medicine community. Claire, who works with Sydney HEMS, delivered an inspiring keynote at the St. Emlyn’s live conference. Her talk focused on excellence, performance, training, and development in retrieval medicine. She emphasized the importance of honesty, feedback, and continuous improvement.
For those aspiring to achieve self-actualization in emergency medicine, Claire’s insights are invaluable. We’ve shared the video and podcast of her talk, and we highly recommend checking them out.
Prognosticating Cardiac Arrest Outcomes: Dan Horner’s Research
Another highlight of January was Professor Dan Horner’s discussion on serum neurofilament light chains, a promising tool for prognosticating cardiac arrest outcomes. This research, stemming from the TTM trial, suggests that these biomarkers can provide early predictions about patient outcomes. Early identification of patients likely to have poor neurological outcomes can significantly impact family discussions, treatment decisions, and overall management.
This research is groundbreaking and holds potential for future clinical applications, although it’s not yet ready for immediate practice.
Celebrating Evidence-Based Medicine: Critical Appraisal E-Book
We’re incredibly proud of our journal club series at St. Emlyn’s, which advocates for evidence-based medicine. This series highlights the latest research, making it accessible and understandable. To celebrate the contributions over the past year, we’ve compiled an e-book available for free download. This resource is a testament to our commitment to advancing medical knowledge and practice.
Pre-Medication for Ketamine Sedation: Exploring New Research
One of the intriguing studies we covered this month examined pre-medication with midazolam or haloperidol for ketamine sedation. The randomized control trial suggested that pre-medication could reduce complications like abnormal behaviors and emergence phenomena. However, it also increased recovery time, requiring more resources and nursing time.
While the findings are interesting, they haven’t convinced us to change our current practice. However, it’s essential to stay informed about such research to make informed decisions in clinical practice.
HEMS and Traumatic Cardiac Arrest: Evaluating Outcomes
We also discussed the role of HEMS in improving outcomes for traumatic cardiac arrest. The study from the UK highlighted the high-level interventions provided by HEMS teams. However, it raised questions about the overall impact on patient survival. Of the 263 patients attended, only seven survived, and all had achieved ROSC before HEMS arrival. This data suggests that while HEMS interventions are critical, their direct impact on survival needs further evaluation.
This topic is sure to spark debate, and we appreciate the transparency of HEMS services in sharing their data and encouraging open discussions.
Looking Ahead: Plans for the Future
As we wrap up January, we’re excited about the plans for the coming months. Simon is heading to Jeddah for a significant event, and we’re considering hosting another St. Emlyn’s live conference and teaching course. We’re exploring innovative formats for medical conferences and welcome your ideas on how we can make these events even more impactful.
Support St. Emlyn’s: Keeping Education Free and Accessible
Since 2012, we’ve funded the blog and podcast out of our own pockets, but as our audience has grown, so have the costs. If you find our content valuable, please consider making a small donation or subscribing for regular contributions. Your support helps us keep St. Emlyn’s free and accessible to all.
Thank you for your time and continued support. Stay tuned for more updates, and as always, enjoy your emergency medicine practice and take care!

Sunday Dec 23, 2018
Ep 125 - November 2018 Round Up
Sunday Dec 23, 2018
Sunday Dec 23, 2018
St Emlyn's November 2018 Review: Key Highlights and Insights
Hello and welcome to the St Emlyn's Podcast and blog. I'm Simon Carley, and I'll be guiding you through the exciting topics and developments we've covered on the blog in November 2018. From leadership insights to groundbreaking medical research, this month has been incredibly informative. Let's dive into the highlights!
Leadership Insights from the FIX Conference
We begin our review in New York, where Natalie May attended the FIX (FeminEM) Conference. In her second post about this event, Natalie explores profound themes, particularly around leadership and motivation in the medical field.
Key Takeaways on Leadership and Motivation
Jennifer Walthall's talk emphasized the importance of acting within the system to drive change. When joining an organization that may not align with your values, you can either work within the system to improve it or fight from the outside. Walthall advocates for influencing change from within, suggesting that once embedded, you can effectively drive improvements.
Lara Goldstein's session on leadership identified four critical attributes of a good leader:
- Listening: Truly understanding your team.
- Recognizing the Impact of Small Actions: Little things add up.
- Conflict Management: Not everyone will like you, and that's okay.
- Gratitude, Kindness, and Decency: Core values that should guide every leader.
Natalie's detailed reflections on the FIX Conference are a must-read for those interested in these themes. Attending FIX in 2019 should be on your list if possible!
POLAR Trial: New Insights into Hypothermia Post-Brain Injury
Dan Horner analyzed the POLAR trial in one of our journal club posts. The POLAR trial is a significant randomized control trial investigating the effects of hypothermia in the early stages after a brain injury. This study follows the Eurotherm trial, which explored hypothermia's role in patients with severe brain injuries in the ICU.
What the POLAR Trial Reveals
The POLAR trial involved 511 patients with severe brain injuries, randomized to either hypothermia (cooling to 33-35°C) or maintaining normothermia for 72 hours. Despite strong pathophysiological evidence supporting hypothermia, the trial found no significant difference in outcomes after six months. Initial results suggest that routine hypothermia for early-stage brain injury might not be beneficial, but long-term data follow-up is crucial. This trial, published in JAMA, is essential reading for anyone involved in emergency medicine or critical care.
The Case for Whole Blood Transfusion in Trauma: Insights from Zaf Qasim
Zaf Qasim, a former Manchester trainee now making waves in the US, contributed an enlightening post on the use of whole blood in trauma resuscitation. This approach, which makes intuitive sense—replacing lost whole blood with whole blood—contrasts with the UK practice of separating blood into components for transfusion.
Advantages of Whole Blood Transfusion
Zaf argues that whole blood could simplify and improve trauma care, reducing the time and complexity of reconstituting blood components in the body. Although not yet standard in the UK, this method is gaining traction in places like London HEMS and various European centers. As data continues to emerge, this could revolutionize trauma care, harkening back to practices from the Second World War and Vietnam.
Challenging the Use of "Sexy" in Clinical Medicine
Natalie May returns with a provocative post challenging the use of the term "sexy" in clinical medicine, especially in resuscitation-related specialties. Often used to describe procedures or equipment, this term can inadvertently perpetuate gender biases and undermine professionalism.
Redefining Professional Language
Natalie, supported by her husband Oli May's humorous yet insightful critique, urges us to reconsider such language. The term "sexy" in a medical context is not a compliment and can contribute to a culture that sexualizes women in the workplace. This reflection is especially relevant for departments striving to maintain professionalism and inclusivity.
Understanding Cognitive Load Theory with Nick Smith
In the realm of medical education, Nick Smith's debut blog post introduces us to cognitive load theory. As a clinical educator in Manchester, Nick explores how intrinsic, extrinsic, and germane cognitive loads affect learning and teaching.
Applying Cognitive Load Theory in Medical Education
Nick's post is a valuable resource for educators aiming to optimize their teaching strategies. By understanding and managing cognitive load, we can create more effective and supportive learning environments for our trainees. This post is part of a broader series on educational theories that are crucial for medical educators.
Elective Experience in South Africa: Lessons from Claire Bromley
Medical student Claire Bromley shares her transformative elective experience at Mitchell's Plain with the BAD EM team. Working with leaders like Katya Evans and Craig Wylie, Claire's reflections offer deep insights into the challenges and rewards of emergency medicine in South Africa.
Bridging UK Training with South African Realities
Claire highlights the stark differences between UK and South African healthcare systems, particularly the intense workload and resource constraints in the public sector. Her experience underscores the importance of preparation, respect, and adaptability for anyone considering working in a different health economy.
Promoting Diversity in the Emergency Department
Natalie May's final post for November reflects on promoting diversity and inclusivity in the emergency department. She emphasizes that the ED is unique in its diversity, seeing patients from all walks of life.
Embracing and Understanding Diversity
Natalie advocates for a broader understanding of diversity beyond ethnicity, including gender, disability, and sexual orientation. Her insights are essential for ED professionals committed to providing equitable care and fostering an inclusive environment.
Learning in the Social Age: Embracing Medutainment
I had the pleasure of discussing "Learning in the Social Age" at the Emerge 10 conference in Scotland. This presentation, supported by a blog post, explores how the internet and social media are transforming medical education.
The Impact of Medutainment
We are now competing on a global scale as educators, with learners accessing information from various sources worldwide. This shift necessitates embracing new methods of engagement, ensuring our teaching remains relevant and impactful.
Beyond ALS: Innovations in Cardiac Arrest Management
We wrapped up November with a highlight from St Emlyn's Live, featuring Salim Rezaie from the RebelEM blog and podcast. Salim's presentation on "Beyond ALS" challenges us to rethink cardiac arrest management, focusing on advanced techniques and evidence-based practices.
Advancing Cardiac Arrest Protocols
Salim's talk covers crucial aspects such as minimizing shock pauses, effective adrenaline administration, and optimizing IV/IO access. For anyone serious about improving their ALS skills, this blog, podcast, and accompanying videos are indispensable resources.
Looking Ahead
November was a whirlwind of activity and learning at St Emlyn's, and we have plenty more in store for December. As we approach the holiday season, we hope you find time to explore these posts and integrate their lessons into your practice. Thank you for being part of the St Emlyn's community, and we look forward to continuing this journey of learning and improvement together.

Sunday Dec 16, 2018
Sunday Dec 16, 2018
This podcast was recorded at the Intensive Care Society State of the Art meeting in London 2018. Simon Carley interviews Prof Peter Brindley on the interface of technology, humans and humanity in critical care. The audio was recorded live and at the venue so there is a fair bit of background noise, but we hope that this does not distract from a wide ranging and fascinating podcast.

Tuesday Nov 13, 2018
Ep 121 - October 2018 Round Up
Tuesday Nov 13, 2018
Tuesday Nov 13, 2018
Welcome to the St Emlyn's Podcast: October 2018 Highlights
Hello and welcome to this St Emlyn’s podcast. My name is Simon Carley, and today I'm thrilled to take you through all the exciting events and updates we've been involved in this October 2018. This month has been bustling with activities, learning opportunities, and insightful experiences that we are eager to share with you.
The Inaugural St Emlyn's Live Conference
We kicked off October with a bang by hosting the first-ever St Emlyn’s live conference in Manchester. This landmark event brought together a diverse group of delegates and speakers, creating a vibrant atmosphere of learning and collaboration. The focus was on the four pillars of emergency medicine as we see it at St Emlyn’s:
- Emergency and Spades Medicine
- Excellence in Critical Care
- Wellbeing
- The Philosophy of Emergency Medicine
We had an incredible day filled with discussions on why we do what we do and how we can continue to improve our practices. The energy and enthusiasm from the participants were palpable, and we are excited to share all the presentations and insights from this event over the coming months. Stay tuned to our blog and media channels for updates.
Five Ways to Improve Your Resuscitation Skills
One of the highlights from the conference was my presentation on "Five Things You Can Do to Improve Your Resuscitation." Although the video is not yet released, the blog post is available, and I want to give you a sneak peek into some practical tips that can make a significant difference in your practice.
1. The Zero Point Survey
The zero-point survey is a concept introduced by Cliff Reid, emphasizing the importance of preparation before patient contact. Your resuscitation process should begin the moment you hear about the patient, not when you meet them. This preparatory phase includes ensuring your physical readiness, team coordination, and environment setup.
Key Steps:
- Self-preparation: Ensure you are physically and mentally ready.
- Team readiness: Identify team roles and confirm competency.
- Environmental setup: Check equipment, ensure visibility, and prepare necessary tools.
2. 10 in 10
The 10 in 10 concept involves taking 10 seconds every 10 minutes during a resuscitation to reassess and communicate with your team. This regular pause helps in reappraising the situation and updating your mental models, ensuring everyone is on the same page.
3. Fly the Patient and Then Think
In emergency medicine, drawing from aviation, one person should focus on maintaining the basics (aviate) while another makes higher-level decisions (navigate and communicate). In a resuscitation scenario, one team member should follow the algorithm and manage immediate life support, while another considers broader strategies and decisions.
4. Peer Review
Peer review is essential for growth and self-awareness. Having someone observe your practice and provide feedback can uncover blind spots and improve your performance. This process benefits both the observer and the observed, fostering a culture of continuous improvement.
5. Hot Debriefs
Adopted from the Edinburgh emergency departments, hot debriefs are quick, five-minute sessions immediately after an event. This practice allows teams to reflect on their performance, discuss what went well, and identify areas for improvement. Implementing hot debriefs can enhance team dynamics and overall performance.
Enhancing Education in Busy Environments
In another educational blog this month, I discussed how to teach and learn effectively in a stretched environment, drawing from a talk at the Royal Society of Medicine in London. Contrary to popular belief, being busy does not preclude learning opportunities. Data from the GMC survey indicates that exposure to relevant cases and support in learning significantly impact trainee satisfaction, rather than workload alone.
Effective Teaching Strategies:
- Post-it Polls: Write down interesting cases or learning points throughout the day and display them on a board for everyone to see and discuss.
- FOAMed Prescriptions: Share relevant online resources with trainees to reinforce learning through spaced repetition.
- Social Media Utilization: Use platforms like WhatsApp and message boards to discuss cases and share insights while maintaining confidentiality.
Cricoid Pressure and RSI: Ongoing Debates
We revisited the controversial topic of cricoid pressure in rapid sequence intubation (RSI) with a journal club post. Despite longstanding debates, recent evidence, including a study published in JAMA, suggests that cricoid pressure may not significantly impact laryngoscopy success rates. However, it might still be beneficial in specific high-risk scenarios. The key takeaway is to make informed decisions based on the latest evidence rather than following traditional practices blindly.
FemInEm Conference Highlights
Natalie May attended the FemInEm conference in New York and shared her insights in a detailed blog post. The FemInEm group focuses on promoting gender equity in emergency medicine but offers valuable resources for all practitioners. Natalie’s presentation on avoiding the use of the word "sexy" in emergency medicine was particularly thought-provoking. Stay tuned for more from this inspiring conference.
Pursuit of Excellence in Emergency Medicine
Natalie May also delivered a keynote presentation at St Emlyn’s Live on the pursuit of excellence. Drawing from her experiences in the UK and Australia, she emphasized the importance of continuous learning and collaboration with colleagues. Her talk highlighted that achieving self-actualization in emergency medicine requires support from a dedicated team, reflection, and a commitment to improvement.
Addressing PTSD in Emergency Medicine
Rusty Carroll continued his series on PTSD, exploring novel therapies such as eye movement desensitization and reprocessing (EMDR), now approved by NICE. This installment provides valuable insights for those dealing with PTSD, offering hope and practical solutions.
Looking Ahead
As we wrap up October, we have an array of exciting content lined up for November and beyond. We will be releasing more materials from St Emlyn’s Live and sharing insights from our Teaching Co-Op course. The course was a fantastic experience, and we are considering hosting it again due to popular demand.
In the meantime, we encourage you to engage with our blogs, videos, and social media channels. Join us in our journey to improve emergency medicine practices and enhance patient care. Stay connected, stay curious, and enjoy your adventures here at St Emlyn’s.
Thank you for being a part of the St Emlyn’s community!
By following these tips and strategies, you can optimize your practice, foster a culture of continuous learning, and improve patient outcomes. Don’t forget to subscribe to our blog and podcast for the latest updates and insights from the world of emergency medicine.

Monday Oct 22, 2018
Ep 119 - September 2018 Round Up
Monday Oct 22, 2018
Monday Oct 22, 2018
September Review: Key Insights from the Sentemlyns Podcast
Welcome to the latest edition of the Sentemlyns podcast blog. I’m Simon Carly, and today we're diving into the significant papers and events from September. We're a tad late this month due to the bustling activities surrounding the Sentemlyns conference and the Teaching Court course, both of which were tremendous successes here in Manchester. Stay tuned as we delve into the highlights of September, from groundbreaking studies to enlightening conferences.
Management of the Airway in Cardiac Arrest
Key Studies by Ashley Levy
We kick off with a comprehensive look at two pivotal papers by Ashley Levy, focusing on airway management in cardiac arrest. These studies, eagerly awaited by the medical community, provide critical insights into pre-hospital care.
Airways 2 Study
Published in JAMA in August, the Airways 2 study examined over 9,000 patients in the UK pre-hospital environment who suffered cardiac arrests. The study excluded patients who quickly returned to spontaneous circulation after a couple of shocks. The remaining patients were randomized into two groups: those receiving a supraglottic airway and those receiving an endotracheal tube.
Findings: The study revealed no significant difference in outcomes between patients who received endotracheal intubation versus those with a supraglottic device. This challenges the long-held belief that intubation is superior in cardiac arrest scenarios.
Implications: The findings suggest that in pre-hospital settings, the choice of airway device might be less critical than previously thought. It underscores the importance of managing ventilation effectively, regardless of the airway device used. For many practitioners, this means opting for the quickest and easiest airway device, typically a supraglottic airway. However, in prolonged or complex cases, converting to an endotracheal tube might still be preferable.
Laryngeal Tube vs. Endotracheal Intubation in the US Study
Another study published in JAMA, conducted in the US, compared endotracheal intubation with the use of a laryngeal tube. Similar to the Airways 2 study, it found no significant advantage to using an endotracheal tube. Interestingly, this study hinted at a slight benefit for the laryngeal tube, though this requires further investigation.
Conclusion: Both studies indicate that for pre-hospital cardiac arrest, the priority should be securing an airway quickly and effectively. While supraglottic airways may suffice in many cases, endotracheal tubes remain a viable option in more complex scenarios.
Global Health and Responsibility
Stefan Brujins’ Perspective
Stefan Brujins, a friend and colleague now working in the UK, provided a thought-provoking post on our responsibilities toward global health. Reflecting on his experiences growing up in South Africa, Stefan challenges us to reconsider our assumptions about equality and diversity in healthcare.
He directs us to an impactful presentation by Annette Alenio at SMACC, emphasizing the need for togetherness in global health. This presentation is a must-watch for anyone interested in global health, offering valuable insights on how we can contribute more effectively to the global medical community.
Highlights from the EUSEM Conference
Diverse Learning Experiences
The EUSEM conference, a combined event with the Royal College of Emergency Medicine, held in Glasgow, was a highlight of September. This event is renowned for its diversity and the unique learning opportunities it offers.
Treatment of Massive PE by Dan Horner
Dan Horner kicked off the conference with an insightful presentation on managing massive pulmonary embolism (PE). His update reflects the latest advancements and the complexities involved in clinical decision-making for thrombolysis in emergency settings. The emphasis on shared decision-making between clinicians and patients was particularly noteworthy.
European Simulation Cup Victory
Members of the Sentemlyns team joined the Royal College of Emergency Medicine team in the European Simulation Cup and emerged victorious. This competition, involving around 14 teams, culminated in a major incident simulation. The win was a testament to the team's skill and collaboration.
Narrative Learning and Storytelling in Emergency Medicine
Simon Carly’s Presentation
I had the opportunity to present on the use of narrative learning and storytelling in emergency medicine. While not a traditional clinical topic, the importance of engaging learners through storytelling cannot be overstated. Case reports, despite being viewed skeptically in literature, remain powerful tools for education when used correctly.
I drew heavily on the work of Jonathan Gottschall, particularly his book "The Storytelling Animal." Understanding the science behind storytelling can transform educational strategies, making them more effective and memorable.
Managing Sick Neonates
Natalie’s Comprehensive Guide
Neonates, with their unique physiology, often present challenges in emergency medicine. Natalie provided an excellent post on managing sick neonates, using the analogy of micro machines to explain various aspects of neonatal care. From glucose metabolism issues to identifying cardiac problems in premature babies, her guide is invaluable for practitioners who may not regularly deal with neonates.
Monkeypox Awareness
Janis Byombi’s Expertise
Monkeypox, a relatively obscure virus related to smallpox, has seen a recent outbreak with cases imported to the UK. Janis Byombi, our expert in international and tropical diseases, detailed the symptoms, diagnosis, and management of monkeypox. While generally self-limiting, awareness and proper handling are crucial, especially for healthcare workers who might be at risk.
RecessTO Conference Insights
Innovative Approaches to Learning
Ashley Liebergen shared her experiences from the RecessTO conference organized by Chris Hicks in Toronto. The conference's innovative approach combined traditional knowledge sharing with practical workshops and simulations, enhancing the overall learning experience. This method of building knowledge progressively throughout the day was particularly effective and engaging.
EMS Gathering in Ireland
Learning with Leisure
The EMS Gathering in Cork, Ireland, offered a unique blend of formal lectures and experiential learning. This “learning with leisure” approach took attendees to various locations around Cork for hands-on experiences, from airport emergencies to extrications.
Emotional Learning Experience One standout session was a cardiac arrest scenario staged in a theatre, focusing on the interaction between medical teams and the patient's relatives. This emotionally charged and theatrically presented scenario highlighted the importance of communication and empathy in emergency medicine.
Zero Point Survey
Enhancing Resuscitation Preparedness
Finally, I rounded off September with a post on the zero-point survey. This concept emphasizes that resuscitation begins before the patient arrives, utilizing the critical minutes from the initial alert to prepare thoroughly. This proactive approach can significantly improve resuscitation outcomes and efficiency.
Conclusion
September was a month of substantial learning and reflection for the Sentemlyns team. From groundbreaking studies in airway management to innovative approaches in global health and emergency medicine education, we've covered a broad spectrum of topics. As we look forward to October and beyond, we remain committed to bringing you the latest insights and developments in emergency medicine.
Thank you for joining us on this journey. Stay tuned for more updates and have a great day!
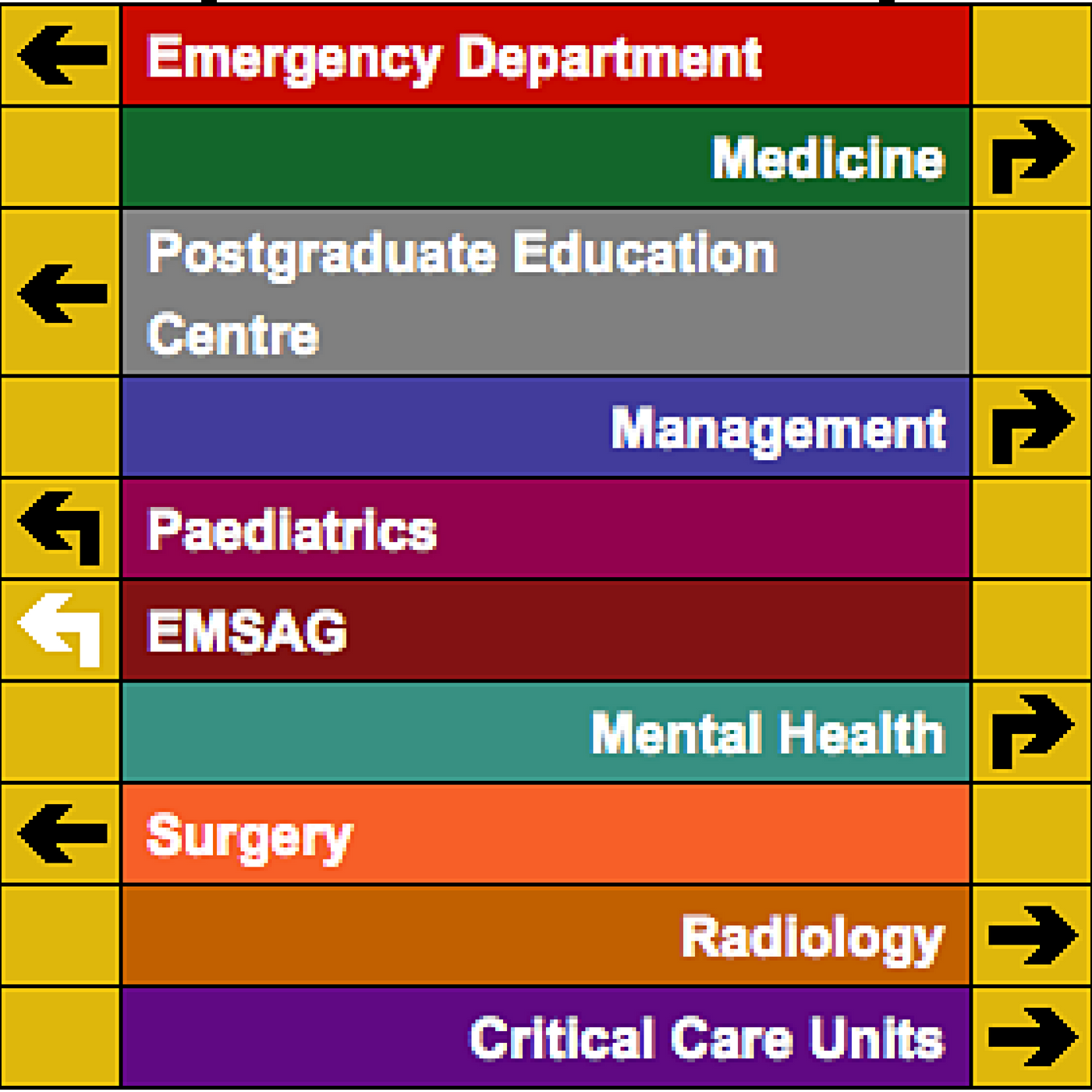
Saturday Jul 21, 2018
Saturday Jul 21, 2018
The Evolution of IV Fluid Therapy: A Critical Review
Welcome to St Emlyn's blog. Today, we explore the evolving landscape of intravenous (IV) fluid therapy in pediatric care. I'm Simon Carly, and I had the privilege of discussing this topic with Dr. Steve Playful at the Royal Manchester Children's Hospital. We delved into the historical context, current practices, and future directions of IV fluid therapy. Here's a comprehensive review of our discussion.
Historical Context of IV Fluids in Pediatrics
The use of IV fluids in pediatrics has undergone significant changes over the years. Approximately 20 years ago, the standard practice involved administering hypotonic fluids to children. This practice was rooted in research from the 1950s that misjudged children's electrolyte and fluid requirements, leading to widespread use of solutions like 0.18% saline with 5% glucose.
However, this approach had its drawbacks. While individual practitioners might not have frequently observed issues, numerous instances of iatrogenic hyponatremia leading to cerebral edema and death highlighted the risks. This spurred a reevaluation of IV fluid therapy practices in pediatrics.
Transition from Hypotonic to Isotonic Solutions
By the late 1990s, concerns about the dangers of hypotonic solutions grew. In 2006, the National Patient Safety Agency in the UK formed a group to address these concerns. They concluded that most children could safely receive half-normal saline as maintenance fluid, except in high-risk situations, marking a significant shift from previous practices.
The pediatric community started adopting isotonic solutions, such as normal saline. However, normal saline (0.9% sodium chloride) presents its own issues. Despite its name, it is not truly "normal" as its sodium content is slightly higher than plasma levels, and its chloride content is about 60% higher. Moreover, the pH of normal saline is around 5.5, far from physiological levels.
Emergence of Balanced Solutions
Balanced solutions have emerged as a promising alternative to both hypotonic and isotonic solutions. Designed to more closely mimic the body's natural plasma, solutions like Ringer's lactate and Plasma-Lyte have gained popularity in the UK. These balanced solutions are buffered with substances like acetate or gluconate to maintain a more physiological pH.
Plasma-Lyte, for instance, is available with and without dextrose, making it versatile for different clinical scenarios. These solutions are typically better tolerated and associated with fewer complications compared to normal saline.
The Debate: Saline vs. Balanced Solutions
The debate over the optimal type of IV fluid for pediatric patients continues. Recent studies, including large international trials, suggest balanced solutions are associated with fewer complications than normal saline. These complications include hyperchloremia, which can lead to acute kidney injury and other adverse outcomes.
Despite these findings, normal saline remains the most commonly administered IV fluid worldwide. This persistence is largely due to tradition and established practices. Changing these deeply ingrained habits requires substantial evidence and updated clinical guidelines.
Key Studies and Evidence
Several studies highlight the benefits of balanced solutions over normal saline. Research indicates that balanced solutions result in less acidosis and fewer chloride level shifts without demonstrated harm. However, not all studies show significant differences. The SPLIT trial, for instance, did not find a marked difference between the two fluid types, though this study had limitations, including uncontrolled pre-enrollment fluid administration and varying severities of illness among patients.
Future Directions in IV Fluid Therapy
As we look ahead, several areas of interest in IV fluid therapy emerge. One key question is which balanced solution is optimal for pediatric patients. Current options include fluids buffered with acetate and gluconate versus those buffered with lactate. Further research is needed to compare these solutions directly.
Another potential development is the inclusion of bicarbonates in balanced solutions. Stabilizing bicarbonates in plastic containers has been challenging, but advances in technology may eventually make this possible, offering a more complete balanced solution.
Practical Recommendations
For clinicians, the decision on which IV fluid to use should be guided by the latest evidence and tailored to the patient's needs. Here are some practical considerations and recommendations:
-
Review the Evidence: Stay informed about the latest research comparing saline and balanced solutions. Reflect on the pathophysiological basis for each type of fluid.
-
Consider the Patient's Condition: For most pediatric patients, balanced solutions are likely safer and more effective. However, specific clinical scenarios may require different approaches. For instance, patients with pyloric stenosis or certain nephrological conditions may benefit from tailored fluid compositions.
-
Monitor and Adjust: Fluid therapy should always be closely monitored and adjusted based on the patient's ongoing needs and responses. This includes considering electrolyte levels, acid-base balance, and overall clinical status.
-
Educate and Advocate: Part of the challenge in shifting to balanced solutions is overcoming established practices and resistance to change. Educate colleagues and advocate for evidence-based practices within your institution.
Conclusion
The evolution of IV fluid therapy in pediatrics mirrors broader trends in medical practice: the quest for safer, more effective treatments, and the need to challenge established norms with new evidence. While much remains to be learned, current evidence strongly supports the use of balanced solutions over traditional saline in most pediatric scenarios.
As clinicians, it's our responsibility to stay informed and adapt practices based on the best available evidence. By doing so, we can improve patient outcomes and advance the field of pediatric medicine.
For those interested in further reading, many of the studies discussed are blogged about on our site. Explore these resources for more detailed discussions and links to original research. Stay informed, stay curious, and continue striving for excellence in your practice.
Thank you for joining us on this deep dive into IV fluid therapy. We hope this discussion has provided valuable insights and practical recommendations for your clinical practice. As always, we welcome your thoughts and feedback on this important topic.

Sunday Apr 29, 2018
Ep 109 - The Physican Response Unit (PRU) with Rich Carden and Tony Joy
Sunday Apr 29, 2018
Sunday Apr 29, 2018
The Physician Response Unit (PRU) is an innovative service in East London that takes the emergency department to the patient. The PRU is led by Tony Joy, consultant in emergency medicine and prehospital care and is a fairly unique service to the UK.
In this podcast our very own Richard Carden interviews Tony for an in depth understanding of how the service is supporting the entire emergency care system in London.
You can read more about the PRU here https://londonsairambulance.co.uk/our-service/news/2017/10/remodelled-pru-to-be-a-seven-day-service-for-the-first-time and look out for a blog post on the St Emlyn's blog site very soon.

Wednesday Jan 24, 2018
Wednesday Jan 24, 2018
Understanding Devastating Brain Injury: Key Insights and Guidelines
In a recent episode of the St Emlyn's podcast, Simon Carley hosted experts Dan Harvey and Mark Wilson to discuss the intricacies of managing devastating brain injury (DBI). The conversation covered new guidelines, the challenges in prognostication, ethical considerations, and practical approaches in clinical settings. This blog post provides a comprehensive summary of their insights, focusing on the importance of standardized care, ethical decision-making, and the role of family involvement.
Defining Devastating Brain Injury
Devastating brain injury encompasses severe brain damage that often leads to significant long-term impairment or death. These injuries can result from various causes, including trauma, subarachnoid hemorrhage, hypoxic brain injury, and intracerebral hematomas. The term "devastating" highlights the severity of these injuries, but as discussed, the perception of devastation can vary, complicating management and prognostication.
The Challenge of Prognostication
One of the core issues in managing DBI is the variability in clinical practice across different healthcare settings. This inconsistency can lead to different outcomes depending on where the patient is treated. Dan Harvey emphasized that the new guidelines aim to standardize care, providing a consistent approach regardless of location. The guidelines recommend an observation period of up to 72 hours to gather comprehensive clinical data, crucial for making informed decisions.
Mark Wilson highlighted the difficulty in early prognostication, noting that initial presentations can be misleading. Factors such as intoxication, medication effects, or pre-existing conditions can obscure the true extent of brain injury. The term "perceived devastating brain injury" underscores the subjective nature of these assessments, stressing that what appears catastrophic on imaging may not always align with clinical outcomes.
The Role of Radiology and Clinical Assessment
Radiological findings, while essential, must be interpreted alongside clinical assessments. A severe CT scan may not always correlate with poor clinical outcomes, and vice versa. The discussion stressed the importance of not rushing to judgment based solely on initial imaging or clinical presentation. Recent studies, including those by Hanni Marcus and Mark Wilson, have shown that some patients with poor prognostic indicators can recover better than expected, particularly those with extra-axial hematomas.
Ethical Considerations and Family Involvement
Ethical considerations are paramount in managing DBI. The definition of a "good recovery" can vary widely among patients and families. For example, elderly patients with significant impairments may still value life, even with extensive care needs. The guidelines emphasize the importance of involving families in discussions about prognosis and treatment, ensuring decisions align with the patient's values and preferences.
Understanding the patient's and family's perspectives is crucial in determining the appropriate course of action. This holistic approach ensures that care decisions are not only medically sound but also ethically and personally appropriate. The discussion also highlighted the need for clear communication, helping families navigate complex and emotionally charged situations.
The Importance of Time and Observation
The guidelines advocate for a period of observation to avoid hasty decisions based on incomplete information. This period, typically up to 72 hours, allows for the identification and management of reversible factors, collection of comprehensive medical history, and better communication with the family. The aim is to reduce the risk of prematurely withdrawing life-sustaining treatment.
Practical Decision-Making
Determining the level of care for DBI patients involves deciding whether to transfer them to neurocritical care units or manage them in general ICUs. While specialized care offers advanced interventions like intracranial pressure (ICP) monitoring, evidence does not conclusively show that these measures always improve outcomes. The discussion acknowledged the limitations of resources and the importance of considering logistical factors, such as proximity to the patient's family.
The guidelines encourage clinicians to make informed decisions based on available evidence and specific case circumstances. They stress that not all DBI patients require transfer to specialized centers, especially when prognosis remains uncertain. The focus should be on providing essential life-saving therapies and monitoring the patient's condition.
Transitioning to Palliative Care
When recovery is deemed unlikely, transitioning to palliative care becomes a compassionate and appropriate choice. The guidelines stress the importance of clear communication with the family, ensuring they understand the prognosis and rationale behind limiting or withdrawing aggressive treatment. Palliative care focuses on symptom management, comfort, and supporting the patient and family, addressing not only physical but also emotional and psychological needs.
Organ Donation Considerations
Organ donation is an important consideration for DBI patients when the prognosis is poor. The guidelines recommend discussing this option with the family as part of end-of-life care planning. These discussions should be handled sensitively, providing clear information and respecting the family's wishes. Organ donation can provide hope and purpose in the face of tragedy, potentially saving other lives.
Conclusion and Key Takeaways
The St Emlyn's podcast episode on devastating brain injury provides crucial insights into the complexities of managing this challenging condition. The newly published guidelines offer a structured approach, emphasizing comprehensive assessment, ethical considerations, and family involvement.
Key Takeaways:
-
Standardize Practice: Reduce variability in DBI management by adhering to standardized guidelines, ensuring consistent and high-quality care.
-
Comprehensive Assessment: Utilize both clinical and radiological assessments to inform prognosis. Avoid premature conclusions based on incomplete data.
-
Ethical and Family Considerations: Engage with families to align treatment decisions with the patient's values and wishes. Provide clear, compassionate communication throughout the process.
-
Observation Period: Allow an appropriate observation period to clarify the patient's condition and potential for recovery.
-
Palliative Care: Transition to palliative care when necessary, prioritizing patient comfort and dignity.
-
Organ Donation: Discuss organ donation as part of end-of-life planning, handling these conversations with care and respect.
By following these guidelines, healthcare professionals can navigate the complexities of managing DBI with greater confidence and compassion, ultimately improving patient outcomes and supporting families through challenging times. For more detailed information and resources, visit the St Emlyn's blog and stay updated with the latest in emergency and critical care.

Friday Oct 06, 2017
Ep 98 - Life as an EM trainee in South Africa. A panel discussion
Friday Oct 06, 2017
Friday Oct 06, 2017
Exploring Emergency Medicine in South Africa: A Journey Beyond the Familiar
Introduction
Hello, and welcome to the St. Emlyn's podcast. I'm Simon Carley, and today, I'm sharing insights from a fascinating experience at the Emergency Medicine Society of South Africa (EMSSA) conference in Sunsetty, Johannesburg. The vibrant city became a backdrop for an enriching exploration into the challenges and rewards of practicing emergency medicine in a vastly different healthcare environment.
This blog post builds on Robert Lloyd's impactful blog about his tough yet enlightening experience at Khayelitsha Hospital. Our journey takes us through candid conversations with UK emergency medicine trainees currently working in South Africa. These discussions reveal not only the clinical and emotional challenges they face but also the profound personal growth they experience.
The Appeal of South African Emergency Medicine
Our conversation begins with a roundtable introduction. Each trainee shares their background and reasons for embarking on this journey. Jen, known as Coffee Headaches on Twitter, is currently working at Khayelitsha Hospital outside Cape Town, having moved from London. Chris and Chloe, both F4s, are working in Benedictine Hospital, Nongoma, and in Malawi, respectively. Sam, Jen's partner, is also at Khayelitsha, while Emma and Jacob, both F5s, are experiencing South African healthcare from different vantage points.
The primary motivation for these trainees to come to South Africa is to gain exposure to cases they rarely see in the UK. This includes a high prevalence of infectious diseases and trauma cases, providing a rich learning environment. The desire to challenge themselves and see how they react in a high-pressure environment is a compelling draw.
Realities of Practicing in South Africa
The conversation quickly shifts to the realities of working in this challenging environment. Despite extensive preparation, the reality of dealing with penetrating trauma, community assaults, and other interpersonal violence in South Africa is stark. As described by Jen and Chris, it's like managing a major incident every weekend night, with a constant flow of young male patients suffering from multiple stab wounds, often brought in by friends or local EMS.
The lack of resources and the necessity to make do with what's available forces a departure from UK-standard protocols. For instance, performing chest drains without the usual monitoring or resources becomes a norm. This scenario is a mental and emotional challenge, as it requires adapting to an environment where the ideal care isn't always possible.
Mental and Emotional Challenges
One of the key discussion points is the mental toll of practising in such a different environment. The trainees express that the most stressful aspect is not being able to provide the level of care they are accustomed to in the UK. The overwhelming number of patients and the lack of resources mean they must often prioritize care based on immediate necessity rather than best practice. This situation requires them to accept that they can't always do everything they would like to, a reality that is difficult to reconcile with their training.
Yet, they also speak of the incredible support network among South African doctors. These professionals guide the UK trainees, helping them navigate the practical challenges and the emotional landscape of emergency medicine in South Africa. This mentorship is invaluable, offering a buffer against the intense stress of the environment.
Unique Clinical Skills and Adaptations
The blog also delves into the unique clinical skills gained in South Africa. Many procedures and techniques, such as the Joburg knot for chest drains, are tailored to the local context, where resources are limited, and patients often face harsher post-treatment conditions. The trainees note that while these methods may not always align with UK standards, they are practical and effective in the South African context.
Moreover, they discuss the necessity of quick decision-making and improvisation. With patients often arriving in critical condition and space at a premium, immediate action is needed, often in less-than-ideal conditions. This experience contrasts sharply with the UK, where procedures are typically performed with more resources and time.
The Emotional Highs and Lows
Despite the challenges, the trainees describe the experience as overwhelmingly positive. The highs of successfully managing complex cases and the lows of resource limitations create a unique learning environment. The exposure to severe trauma cases, particularly penetrating injuries, has significantly reduced their anxiety about these scenarios. This newfound confidence is something they plan to bring back to their practice in the UK.
The trainees also express deep admiration for their South African colleagues, who demonstrate remarkable skill and resilience in a resource-limited setting. The ability of these professionals to provide high-quality care despite significant challenges is both inspiring and humbling.
Recommendations for Future Trainees
As the discussion winds down, the trainees share advice for others considering similar experiences. They emphasize the importance of understanding the expectations and conditions of the placement. The experiences can vary widely depending on whether one ends up in a well-supported trauma unit in a city or a rural hospital with minimal resources and support.
They recommend a minimum stay of three months to truly understand and contribute effectively to the healthcare setting. Shorter stays, they argue, don't provide enough time to adapt to the environment or make a meaningful impact.
Conclusion
Our conversation concludes with a reflection on the broader implications of this experience. The trainees agree that the skills and resilience developed in South Africa are not only invaluable but also applicable to emergency medicine practice in the UK. The experience underscores the need for adaptability, resourcefulness, and a deep understanding of the human aspects of healthcare.
South Africa, with its unique challenges and vibrant culture, offers an unparalleled learning experience for emergency medicine trainees. The personal and professional growth that comes from working in such a diverse and demanding environment is immense. As the trainees prepare to return to the UK, they carry with them not only new clinical skills but also a deeper understanding of themselves as clinicians.
This experience has been a powerful reminder that the essence of emergency medicine transcends geographical and cultural boundaries. It's about providing the best possible care under any circumstances, a lesson that resonates deeply with the core values of St. Emlyn's.
If you're considering a similar journey, take the plunge. The highs and lows are part of a journey that will not only shape your medical career but also broaden your perspective on healthcare and humanity. As we say goodbye to South Africa, the stories and lessons from this experience will undoubtedly inspire and inform the future of emergency medicine practice, both in the UK and beyond.

Wednesday Mar 22, 2017
Ep 90 - Top Ten Trauma Papers 2016
Wednesday Mar 22, 2017
Wednesday Mar 22, 2017
In this episode of the St Emlyn's podcast, Ian Beardsell and Simon Carley review the top 10 trauma papers of the year, highlighting key findings and their implications for trauma care. The selection includes significant studies published in high-profile journals such as The Lancet and the New England Journal of Medicine, offering valuable insights for healthcare professionals in emergency and trauma medicine.
1. Whole Body CT Scanning: REACT-2 Study
The REACT-2 study explored the impact of whole-body CT (WBCT) scanning on trauma patients, particularly its effect on mortality rates. The study involved 1400 patients and found no significant difference in mortality between those who received WBCT and those who underwent more selective CT scanning. The difference in radiation exposure was minimal, suggesting that WBCT's comprehensive imaging might be more beneficial than harmful, especially in elderly patients where missed injuries can complicate outcomes. This study reassures trauma team leaders that current scanning practices are appropriate and highlights the importance of a patient-centred approach based on clinical presentation.
2. Impact Brain Apnea (IBA)
Impact brain apnea, characterized by apnea and a catecholamine surge following a severe head blow, has been increasingly recognized in trauma care. The paper, co-authored by John Hines and Mark Wilson, provides a detailed explanation of IBA's pathophysiological mechanisms. This condition can lead to cardiac arrest if not promptly addressed, emphasizing the need for immediate intervention in cases of traumatic brain injury (TBI). Understanding IBA helps emergency care providers identify and treat potentially life-threatening conditions that may not be immediately apparent.
3. Decompressive Craniectomy for Raised ICP: RESCUE-ICP Trial
The RESCUE-ICP trial examined the outcomes of decompressive craniectomy in patients with refractory intracranial pressure (ICP) due to severe TBI. The study found that while the procedure increased survival rates, many survivors experienced significant disability. This raises ethical considerations about the quality of life post-intervention. The trial underscores the importance of informed consent and discussions about potential outcomes with patients' families, aligning treatment with patient values.
4. STITCH Trial: Surgery Timing for Intracranial Bleeds
The STITCH trial focused on the timing of surgical intervention in patients with traumatic intracranial bleeds. Although the trial faced recruitment challenges and was terminated early, results suggested better outcomes with early surgery. This finding, while not statistically conclusive, supports the notion that timely intervention can reduce mortality and improve recovery. Emergency physicians and neurosurgeons should consider these findings when deciding on surgical timing in TBI cases.
5. Traumatic Cardiac Arrest: Epidemiology and Outcomes
Using data from the Trauma Audit and Research Network (TARN), this study examined traumatic cardiac arrest (TCA) cases, revealing a 30-day survival rate of 7.5%. This rate, similar to medical cardiac arrests, challenges the perception that TCA is almost always fatal. The study highlights the importance of aggressive resuscitation efforts and underscores the need for ongoing training to retain skills in managing these rare but critical events.
6. Open vs. Closed Chest Compressions in TCA
The effectiveness of open chest (thoracotomy) versus closed chest compressions in TCA was explored, with findings indicating similar outcomes in terms of end-tidal CO2 levels, a marker for effective CPR. This challenges the notion that thoracotomy should always be performed in TCA cases. The study suggests that standard advanced life support (ALS) protocols may suffice in certain scenarios, especially where thoracotomy is not practical.
7. Rocuronium vs. Succinylcholine for RSI in Severe Brain Injury
The choice between rocuronium and succinylcholine for rapid sequence intubation (RSI) in severe brain injury remains debated. An observational study found no significant overall difference in mortality between the two drugs, though succinylcholine was associated with higher mortality in severe head injury cases. This suggests a possible preference for rocuronium in such scenarios, though the evidence is not strong enough to mandate a change in practice.
8. Intraosseous Needle Length in Obese Patients
As obesity becomes more prevalent, appropriate intraosseous (IO) needle length is crucial for effective vascular access. The study recommended using longer yellow IO needles for patients with a BMI over 43, as standard blue needles may not reach the marrow. This is particularly important in emergency situations where IV access is difficult, ensuring proper drug administration and preventing complications like compartment syndrome.
9. Optimal Site for Needle Decompression in Tension Pneumothorax
A systematic review recommended the anterior axillary line as the preferred site for needle decompression in tension pneumothorax, aligning with standard chest drain placement. The review also noted significant complication rates associated with needle decompression, suggesting that alternative methods like thoracostomy may be necessary in certain cases. This finding emphasizes the need for precise technique and careful consideration in managing tension pneumothorax.
10. Weekend Effect in Major Trauma Care
The study examined the "weekend effect" in major trauma care, finding no significant difference in mortality between weekend and weekday admissions. This suggests that well-resourced, consultant-led trauma care can provide consistent outcomes regardless of the day. The findings advocate for the 24/7 availability of senior emergency physicians and trauma teams, ensuring high-quality care at all times.
Conclusion
This year's top trauma papers provide valuable insights into current practices and emerging trends in trauma care. While there may not have been groundbreaking changes, the studies reinforce the importance of evidence-based decision-making, ongoing training, and ethical considerations in patient management. As the field evolves, staying informed about the latest research is crucial for improving patient outcomes and delivering high-quality trauma care. For further details and access to the studies, visit the Sentemlin site and related FOAMed resources.

Tuesday Feb 14, 2017
Ep 88 - ED transfers. Patient, Preparation and People.
Tuesday Feb 14, 2017
Tuesday Feb 14, 2017
Nat and Simon discuss the complexities of transferring a patient from the resus room to CT and back again. Look out for the blog post soon on stemlynsblog.org

Tuesday Dec 13, 2016
Ep 85 - Top tips for chest drains.
Tuesday Dec 13, 2016
Tuesday Dec 13, 2016
Title: Mastering Chest Drains: Essential Tips and Techniques for Emergency Medicine
In this comprehensive guide, Simon Carley and Rick Bodey from St Emlyns explore the essential aspects of chest drains, also known as intercostal drains or chest tubes, focusing on their importance, optimal techniques, and common pitfalls in emergency medicine.
Importance of Chest Drains
Chest drains are critical for managing conditions like pneumothorax, hemothorax, and pleural effusion by removing air, blood, or fluid from the pleural cavity. Despite not being a daily procedure in the UK, proficiency in chest drain insertion is crucial due to the potential for severe complications, including organ damage and infection. Proper training and careful execution are necessary, especially as new technologies and medical practices evolve.
Choosing the Right Size
Traditionally, large-bore drains (32-36 French) were used for pneumothoraces to prevent blockage by clots. However, recent evidence supports the use of smaller drains (28-32 French), even for trauma patients. Smaller drains are less invasive, cause less discomfort, and are equally effective. The move towards smaller drains aligns with a trend in medicine favoring minimally invasive procedures, which reduce patient risk and enhance comfort.
Management of Occult Pneumothoraces
Advances in imaging, like CT scans and ultrasound, have increased the detection of occult pneumothoraces, which are often asymptomatic and not visible on chest x-rays. Traditional guidelines recommended chest drains for all traumatic pneumothoraces, but recent research suggests conservative management may be appropriate in many cases. A systematic review found no significant difference in outcomes between patients with occult pneumothoraces managed conservatively and those who received chest drains. This highlights the importance of assessing each patient's condition, monitoring closely, and only intervening when necessary, particularly in stable, asymptomatic patients.
Optimizing Analgesia
Pain management during chest drain insertion is vital. Traditional local anesthesia methods are often insufficient, especially in trauma settings. Ketamine has emerged as an effective option, providing both analgesia and sedation without significant respiratory depression. Administered in small, incremental doses, ketamine helps manage pain and anxiety, making the procedure more tolerable. Additional analgesics, like fentanyl and midazolam, can complement ketamine, offering a multimodal approach to pain management.
Intra-Pleural Analgesia
Injecting local anesthetics, such as bupivacaine, into the pleural cavity can further enhance patient comfort, particularly as the lung re-expands and contacts the parietal pleura. This method is supported by randomized controlled trials and can significantly reduce pain in the first few hours post-insertion, aiding in better respiratory function and reducing the risk of complications like pneumonia.
Securing the Drain
Properly securing the chest drain is crucial to prevent accidental dislodgement, especially during patient transport or imaging. Techniques like Neil Bandari's "Jo'burg knot" offer reliable methods for securing drains, though simpler techniques may suffice for less frequent practitioners. Transparent dressings are recommended to allow monitoring of the insertion site and ensure the drain remains securely anchored.
The Role of Ultrasound
Ultrasound is an invaluable tool for accurately placing chest drains, particularly in cases of pleural effusion or complex pleural anatomy. It aids in identifying the best insertion site, reducing the risk of complications, and confirming the resolution of pneumothorax. Ultrasound is especially useful in patients with obesity or chronic lung conditions, where traditional landmarks may not be reliable.
Aspiration of Pneumothoraces
For primary spontaneous pneumothoraces, aspiration may be a viable alternative to chest drain insertion, particularly when specific criteria are met. This less invasive approach can be performed with a standard IV cannula or a small Seldinger technique, which also provides a pathway for chest drain insertion if necessary. This method is beneficial in outpatient settings, allowing for quick resolution without hospitalization.
Conclusion
The management of chest drains is a dynamic field, continually evolving with new research and technology. Emergency medicine practitioners must stay informed and adapt to evidence-based practices, including the use of smaller chest drains, conservative management of occult pneumothoraces, optimized analgesia, and the application of ultrasound. The goal is to provide safe, effective, and patient-centered care, minimizing unnecessary interventions.
At St Emlyns, we strive to share knowledge and best practices to enhance patient care. We invite our readers to contribute their insights and experiences, fostering a collaborative approach to improving clinical skills and outcomes in emergency medicine.

Wednesday Oct 12, 2016
Ep 81 - Difficult Conversations with Children in Critical Care with Liz Crowe
Wednesday Oct 12, 2016
Wednesday Oct 12, 2016
Helping Children Understand Tragedy: Guidance for Parents and Professionals
In a recent St Emlyn's podcast, Iain Beardsell and Liz Crowe, an advanced social worker in a pediatric intensive care unit in Brisbane, explored the critical topic of how to communicate with children during tragic situations. The discussion emphasized the importance of honesty and directness when dealing with topics like illness, death, and other forms of hardship.
Understanding the Context
Historically, children in many cultures were more regularly exposed to the realities of life, such as birth and death. In contrast, modern Western societies often shield children from these experiences. However, Liz asserts that children are more perceptive and resilient than we give them credit for, and attempts to protect them from all emotional pain can be detrimental. Shielding children from the truth can lead to confusion and increased anxiety, as they often sense when something is wrong, even if it is not explicitly communicated to them.
The Importance of Honesty
When difficult situations arise, such as a family member being diagnosed with a serious illness or being involved in an accident, adults may feel the instinct to protect children by withholding information. However, research and experience show that children cope better when they are informed and involved. Children, especially those under ten, can mistakenly believe they are responsible for negative events due to their egocentric worldview. Therefore, it is crucial to communicate clearly and truthfully, helping them understand the situation without assigning blame to themselves.
Balancing Protection and Reality
Parents naturally want to protect their children from pain. However, overprotection can prevent children from learning to deal with disappointment and hardship, essential components of developing resilience. Liz argues that by being overly protective, we may contribute to rising rates of depression and mental health issues among young people. It's essential to prepare children for life's challenges by allowing them to experience and understand difficult emotions in a supportive environment.
Practical Approaches to Communication
When faced with the need to communicate difficult news to children, it's important to empower familiar adults—such as parents or guardians—to have these conversations rather than leaving them to strangers. Here’s a suggested approach:
- Preparation: Prepare the adults involved in the child's life by discussing the importance of honest communication and the possible impacts of the conversation.
- Setting Expectations: Describe what the child might see, hear, and feel to reduce anxiety and set clear expectations.
- Use Specific Language: Avoid euphemisms. Use specific medical terms like "neuroblastoma" or "head injury" to describe the situation accurately.
- Timing and Environment: Choose an appropriate time and setting for the conversation, avoiding moments when the child might be tired or distracted.
- Stick to the Facts: Provide clear, factual information without overwhelming the child. Keep explanations straightforward and allow time for processing.
- Encourage Questions: Allow the child to ask questions and answer them honestly. It’s okay to admit if you don’t have all the answers.
- Ongoing Support: Be available for follow-up conversations, as children may revisit these topics as they process the information.
Using Accurate Language
It’s crucial to use accurate language when discussing severe issues. Avoid using vague terms like "poorly," which can lead to misunderstandings. For example, describing a child as "very sick" without specifying the illness can cause confusion and fear, especially if the child later associates the term with less severe conditions. Using specific medical terminology helps children differentiate between different types of illnesses and their severity.
Long-Term Impact on Children
Many parents and caregivers worry that exposure to tragedy will permanently damage their children. While such experiences can indeed be life-changing, they do not necessarily result in negative outcomes. Children who experience the death of a sibling or parent may grieve and feel pain, but they can also develop greater empathy and understanding of life's complexities. Research indicates that while children in these situations may have higher levels of anxiety, they are not necessarily less successful academically or socially. They often develop a deeper sensitivity and a better understanding of life.
The Role of Counseling and Support
While counseling can be helpful, Liz cautions against making it the default response. Instead, she suggests that families should be encouraged to navigate these challenges on their own, seeking professional help only if they find themselves unable to cope. This approach fosters resilience and self-reliance, teaching children that while therapy is a valuable resource, it's not always necessary.
Conclusion: Building Resilience
Ultimately, difficult conversations with children about tragedy are a necessary part of life. By approaching these conversations with honesty, clarity, and support, we can help children navigate their emotions and develop the resilience needed for future challenges. Whether as parents or healthcare professionals, our role is to guide children through these experiences, providing the tools and understanding they need to grow and thrive.
At St Emlyn's, we believe that while we can't shield children from all of life's difficulties, we can help them face these challenges with courage. The experiences that children go through, even the painful ones, can serve as opportunities for growth and learning. With the right support, children can emerge from these experiences stronger and better equipped to handle life's complexities. Our goal is to create a safe space for children to express their feelings, ask questions, and ultimately, develop the resilience they need to navigate the ups and downs of life

Thursday Feb 04, 2016
Ep 65 - The management of Paediatric trauma in the UK with Ross Fisher
Thursday Feb 04, 2016
Thursday Feb 04, 2016
Ross Fisher, consultant paediatric surgeon and lead for TARNlet joins Simon Carley at the London Trauma Conference to discuss the challenges in managing paediatric trauma in the UK.

Wednesday Dec 30, 2015
Ep 62 - The role of paediatric surgeons in trauma with Ross Fisher (LTC)
Wednesday Dec 30, 2015
Wednesday Dec 30, 2015
Simon and Ross Fisher from Sheffield discuss the emerging role of paediatric surgeons in trauma. This podcast was recorded at the London Trauma Conference (so sorry for a bit of background noise at times).
vb
S
Wednesday May 06, 2015
Ep 46 - Intro to EM: The patient with asthma
Wednesday May 06, 2015
Wednesday May 06, 2015
Introduction
Welcome to the St. Emlyn's induction podcast recap, where we dive deep into the management of asthma in the emergency department. Asthma is a prevalent condition that emergency medical professionals encounter frequently. This blog post will provide a detailed step-by-step guide to managing patients presenting with asthma, including case presentation, assessment, treatment, and discharge planning. Whether you're a seasoned practitioner or new to emergency medicine, this guide aims to enhance your understanding and improve patient outcomes.
Case Presentation: Recognizing Severe Asthma
Imagine you're in the resuscitation room when you're alerted about an incoming patient. A 30-year-old female with a history of acute severe asthma is being brought in. She's a smoker, consuming 20 cigarettes a day, and has had a history of hospital admissions, including an ICU stay a few years ago. As she is wheeled in, you notice she is short of breath with audible wheezing. This initial presentation provides critical information for immediate action.
First Steps: Rapid Assessment and Initial Management
Upon the patient's arrival, it's crucial to make a rapid assessment. Conducting an ABC (Airway, Breathing, Circulation) assessment is essential to confirm the diagnosis and gauge the severity of the asthma attack. Given the patient's severe condition, it's vital to start treatment immediately while continuing your assessment.
Immediate Actions
- High-Flow Oxygen: Administer high-flow oxygen to improve oxygen saturation levels.
- Nebulizers: Start with 5 mg of salbutamol and 500 mcg of ipratropium bromide. Don't hesitate to administer another dose if needed.
- Listen to the Chest: A quick auscultation of the chest can help confirm the presence of wheezes and rule out other conditions like tension pneumothorax.
Understanding the Severity of Asthma
Assessing the severity of asthma is critical to guiding further treatment. The British Thoracic Society provides guidelines that classify asthma into mild, moderate, acute severe, and life-threatening categories.
Criteria for Severity
- Mild Asthma: Patients might experience mild dyspnea but can generally manage with minimal intervention.
- Moderate Asthma: Characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable at home with proper medication.
- Acute Severe Asthma: Marked by a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences.
- Life-Threatening Asthma: Includes a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion.
Continuous Management: Treating Severe Asthma
In cases of severe or life-threatening asthma, continuous management and close monitoring are paramount.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Use salbutamol and ipratropium bromide back-to-back to provide relief.
Steroid Administration
Steroids play a crucial role in managing asthma by reducing inflammation. Administer oral steroids (1-2 mg/kg of prednisolone) or intravenous steroids if oral administration is not feasible.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it's available when needed.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel.
Additional Therapies
- Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma.
- CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress.
Importance of Senior Support
It's vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available.
Discharge Planning: Ensuring Safe Transition
For patients showing improvement, careful discharge planning is essential to prevent relapse and ensure ongoing management.
Criteria for Discharge
- Stability: Ensure the patient is stable for at least 6-8 hours after initial treatment.
- Follow-Up: Arrange follow-up with a general practitioner or asthma nurse within a few days.
- Medication Review: Ensure the patient has access to their inhalers and understands their use.
- Safety Netting: Advise the patient to return if symptoms worsen, even if they are already on their way home.
Safety Measures
Natalie May from St. Emlyn's emphasizes the importance of advising patients to return if they have any concerns, even after leaving the hospital. Ensuring patients have their therapy and understand their treatment plan is crucial for safe discharge.
Conclusion: Recap and Key Takeaways
In summary, managing asthma in the emergency department requires a systematic approach:
- Rapid Assessment: Quickly assess the severity using ABC and confirm the diagnosis.
- Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
- Continuous Management: Use back-to-back nebulizers, steroids, and consider IV bronchodilators and magnesium sulfate.
- Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
- Discharge Planning: Ensure the patient is stable, arrange follow-up, review medications, and provide safety netting advice.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
Further Resources
For more detailed information, refer to the British Thoracic Society guidelines and explore additional induction podcasts available on iTunes. Staying updated with the latest research and best practices is essential for improving patient outcomes in asthma management.
References
- British Thoracic Society Guidelines
- St. Emlyn's Induction Podcasts
- Recent Studies on Magnesium Sulfate in Asthma Management
Keywords
- Asthma management
- Emergency department
- Severe asthma
- Life-threatening asthma
- High-flow oxygen
- Nebulizers
- Salbutamol
- Ipratropium bromide
- Steroids in asthma
- Intravenous bronchodilators
- Magnesium sulfate
- Critical care in asthma
- CPAP in asthma
- Ketamine infusion
- Asthma discharge planning
By following these guidelines and staying informed, healthcare professionals can effectively manage asthma in emergency settings, ensuring the best possible outcomes for their patients.
Recognizing and Managing Severe Asthma in the Emergency Department: A Detailed Guide
Asthma is a common condition frequently encountered in emergency departments. Managing patients presenting with asthma, particularly those with severe symptoms, requires a systematic and prompt approach. This guide will focus on the initial assessment and management steps for a patient presenting with severe asthma in the emergency department, providing detailed insights into immediate actions and the rationale behind them.
Case Presentation: Recognizing Severe Asthma
Consider a typical scenario in the resuscitation room. You receive an alert about a 30-year-old female with a history of acute severe asthma. This patient, a smoker who consumes 20 cigarettes a day, has previously been admitted to the ICU for asthma-related issues. She is brought in, visibly short of breath and with an audible wheeze.
This initial presentation is critical for immediate action. Recognizing the signs of severe asthma and understanding the patient's history sets the stage for effective management.
Initial Management: Rapid Assessment and Treatment
Upon the patient's arrival, a rapid assessment is essential. Conducting an ABC (Airway, Breathing, Circulation) assessment helps confirm the diagnosis and determine the severity of the asthma attack. Given the patient's severe condition, simultaneous assessment and treatment are necessary.
Immediate Actions
-
Administer High-Flow Oxygen: The first step is to administer high-flow oxygen. This intervention aims to improve the patient's oxygen saturation levels, which is crucial for stabilizing their condition.
-
Start Nebulizers: Administer a combination of 5 mg of salbutamol and 500 mcg of ipratropium bromide. These medications help relax the bronchial muscles and reduce bronchospasm. If the patient remains symptomatic, additional doses can be given without hesitation.
-
Listen to the Chest: A quick auscultation of the chest can confirm the presence of wheezes and rule out other conditions, such as a tension pneumothorax. This step ensures that the treatment plan is appropriate and targeted.
Understanding Asthma Severity
Assessing the severity of asthma is crucial for guiding treatment decisions. The British Thoracic Society's guidelines classify asthma into mild, moderate, acute severe, and life-threatening categories based on specific clinical criteria.
Severity Criteria
-
Mild Asthma: Patients with mild asthma may experience mild dyspnea and can usually manage with minimal intervention.
-
Moderate Asthma: This category is characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable with proper medication at home.
-
Acute Severe Asthma: Patients in this category have a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences. Immediate and aggressive treatment is required.
-
Life-Threatening Asthma: This is marked by a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion. These patients require urgent and intensive intervention.
Continuous Management: Treating Severe Asthma
For patients with severe or life-threatening asthma, continuous management and close monitoring are essential.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Salbutamol and ipratropium bromide should be given back-to-back to provide maximum relief.
Steroid Administration
Steroids are crucial in managing asthma by reducing inflammation. Administer oral steroids, such as 1-2 mg/kg of prednisolone, or intravenous steroids if oral administration is not feasible. While steroids do not provide immediate relief, they help reduce the underlying inflammation and prevent future exacerbations.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it is available when needed.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients. However, it should not delay other critical treatments.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel.
Additional Therapies
-
Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma.
-
CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress.
Importance of Senior Support
It is vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available.
Discharge Planning: Ensuring Safe Transition
For patients showing improvement, careful discharge planning is essential to prevent relapse and ensure ongoing management.
Criteria for Discharge
-
Stability: Ensure the patient is stable for at least 6-8 hours after initial treatment.
-
Follow-Up: Arrange follow-up with a general practitioner or asthma nurse within a few days.
-
Medication Review: Ensure the patient has access to their inhalers and understands their use.
-
Safety Netting: Advise the patient to return if symptoms worsen, even if they are already on their way home.
Safety Measures
Natalie May from St. Emlyn's emphasizes the importance of advising patients to return if they have any concerns, even after leaving the hospital. Ensuring patients have their therapy and understand their treatment plan is crucial for safe discharge.
Conclusion: Recap and Key Takeaways
In summary, managing asthma in the emergency department requires a systematic approach:
-
Rapid Assessment: Quickly assess the severity using ABC and confirm the diagnosis.
-
Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
-
Continuous Management: Use back-to-back nebulizers, steroids, and consider IV bronchodilators and magnesium sulfate.
-
Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
-
Discharge Planning: Ensure the patient is stable, arrange follow-up, review medications, and provide safety netting advice.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
By following these guidelines and staying informed, healthcare professionals can effectively manage asthma in emergency settings, ensuring the best possible outcomes for their patients.
First Command: Initial Management of Severe Asthma in the Emergency Department
Asthma is a common, chronic respiratory condition that often presents acutely in emergency departments. Managing a severe asthma attack requires immediate and decisive action to prevent life-threatening complications. This guide will walk you through the first command in the management of severe asthma: recognizing the severity of the condition and initiating appropriate treatment promptly.
Case Scenario
Picture yourself in the resuscitation room when you receive an alert about a patient en route to the hospital. The patient is a 30-year-old female with a history of acute severe asthma. She is a 20-a-day smoker and has had previous hospital admissions, including a stay in the Intensive Care Unit (ICU) a few years ago. Upon her arrival, she is visibly short of breath with an audible wheeze.
Immediate Assessment and Treatment
Upon the patient's arrival, it is critical to make a rapid assessment and initiate treatment simultaneously. The goals are to confirm the diagnosis, assess the severity of the asthma attack, and begin interventions that can stabilize the patient.
Rapid Assessment: ABC Approach
-
Airway: Ensure the airway is clear. Asthma patients typically do not have airway obstructions, but it is crucial to check for any foreign bodies or swelling that might complicate the condition.
-
Breathing: Assess the patient's breathing. Look for signs of respiratory distress, such as rapid breathing, use of accessory muscles, and the presence of wheezing. Measure oxygen saturation using a pulse oximeter.
-
Circulation: Check the patient's heart rate and blood pressure. Asthma can cause tachycardia and hypertension due to the stress of breathing difficulties.
Initial Actions
-
Administer High-Flow Oxygen: The first and most crucial step is to administer high-flow oxygen. This intervention aims to improve the patient's oxygen saturation levels. Use a non-rebreather mask to deliver a high concentration of oxygen (usually 15 liters per minute).
-
Start Nebulizers: Administer bronchodilators through a nebulizer. Begin with 5 mg of salbutamol and 500 mcg of ipratropium bromide. These medications help to relax the bronchial muscles and reduce bronchospasm, facilitating easier breathing. If the patient remains symptomatic, additional doses can be administered without hesitation.
-
Listen to the Chest: Perform a quick auscultation of the chest to confirm the presence of wheezes and rule out other conditions such as a tension pneumothorax. The presence of bilateral wheezing supports the diagnosis of an asthma exacerbation.
Understanding Asthma Severity
Assessing the severity of the asthma attack is essential for guiding treatment decisions. The British Thoracic Society classifies asthma into mild, moderate, acute severe, and life-threatening categories based on specific clinical criteria.
Severity Criteria
-
Mild Asthma: Patients with mild asthma may experience mild dyspnea and can usually manage with minimal intervention.
-
Moderate Asthma: Characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable with proper medication at home.
-
Acute Severe Asthma: Patients in this category have a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences. Immediate and aggressive treatment is required.
-
Life-Threatening Asthma: Marked by a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion. These patients require urgent and intensive intervention.
Continuous Management: Treating Severe Asthma
For patients with severe or life-threatening asthma, continuous management and close monitoring are essential.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Salbutamol and ipratropium bromide should be given back-to-back to provide maximum relief. This approach ensures that the bronchodilators maintain their effect, reducing airway resistance and improving airflow.
Steroid Administration
Steroids play a crucial role in managing asthma by reducing inflammation. Administer oral steroids, such as 1-2 mg/kg of prednisolone, or intravenous steroids if oral administration is not feasible. While steroids do not provide immediate relief, they help reduce the underlying inflammation and prevent future exacerbations.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it is available when needed. Intravenous administration allows the medication to reach the target sites quickly, providing more effective relief in severe cases.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients. However, it should not delay other critical treatments.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel. Early involvement of critical care can facilitate the management of severe cases and improve patient outcomes.
Additional Therapies
-
Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma. It provides sedation and bronchodilation, which can be beneficial in severe cases.
-
CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress. It helps to keep the airways open and reduce the work of breathing.
Importance of Senior Support
It is vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available. Senior clinicians can provide guidance on advanced therapies and ensure that all possible interventions are considered.
Conclusion: Recap and Key Takeaways
Managing severe asthma in the emergency department requires a systematic and prompt approach:
-
Rapid Assessment: Quickly assess the severity using the ABC approach and confirm the diagnosis.
-
Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
-
Continuous Management: Use back-to-back nebulizers, steroids, and consider intravenous bronchodilators and magnesium sulfate.
-
Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
By following these guidelines, healthcare professionals can effectively manage severe asthma in emergency settings, ensuring the best possible outcomes for their patients.

Monday Apr 27, 2015
Ep 45 - Top 10 trauma papers 2014-2015.
Monday Apr 27, 2015
Monday Apr 27, 2015
A first podcast with Simon Laing from the RCEMFOAMed team. We look back at influential trauma related papers from 2014-2015.

Saturday Apr 18, 2015
Ep 44 - Tim Draycott on Obstetric Trauma (LTC 2014)
Saturday Apr 18, 2015
Saturday Apr 18, 2015
Iain interviews the wonderful Tim Draycott on the management of the Obstetric patient with trauma.Tim is a consultant Obstetrician from Bristol and is a great speaker on this rather terrifying topic!

Thursday Mar 26, 2015
Ep 43 - APLS 2015 updates for the management of the serious injured child
Thursday Mar 26, 2015
Thursday Mar 26, 2015

A short podcast updating the UK Advanced Paediatric Life Support (APLS) course guidelines for the management of trauma in children.
Don't forget to read the blog post here. APLS Updates: New kids on the block,
vb
S

Wednesday Dec 03, 2014
Ep 28 - Iain and Nat preview the amazing London Trauma Conference.
Wednesday Dec 03, 2014
Wednesday Dec 03, 2014
Exciting Collaboration Between St Emlyns and the London Trauma Conference
Welcome to the latest St Emlyns podcast! I'm Iain Beardsell, and alongside Natalie Mace, we are thrilled to announce an exciting new collaboration between the St Emlyns team and the London Trauma Conference. This esteemed conference will take place in London next week, and we've been honored with the opportunity to attend as members of the press. We will be interviewing some of the prominent speakers participating in the event, marking a significant first for our team at St Emlyns.
The London Trauma Conference: Dates and Highlights
The London Trauma Conference is scheduled from Tuesday, December 9th to Thursday, December 11th. This three-day event promises a stellar lineup of speakers from the Trauma World, including sessions on Trauma Surgery, Trauma Nursing, and a dedicated day for trainees. There’s even a special Thoracotomy day planned. This comprehensive program ensures there’s something for everyone in the field of trauma care.
Why Attend the London Trauma Conference?
We are not just attending to listen; our goal is to bring you the inside stories and insights from the speakers after their sessions. We aim to ask the questions you want answers to, making this conference more interactive and engaging for all of us. Whether you are a seasoned professional or a trainee, this conference offers invaluable knowledge and networking opportunities.
If you’re considering attending, we highly encourage it. You can find all the details and register at www.londontraumaconference.com. There are still places available, so don’t miss out on this exceptional event.
Engaging with the Conference Online
For those who can't make it to London, there are still plenty of ways to stay involved. Follow along on Twitter using the hashtag #ltc2014. We will be tweeting live updates from the sessions, and you can tweet your questions to us. We’ll do our best to catch up with the speakers and get your questions answered.
Getting Ready for Trauma Week
To get in the mood for the upcoming trauma week, we recommend listening to "The Fight for Life," a program by Kevin Fong on BBC Radio 4. This enlightening show traces the origins of trauma care and brings it up to the modern day. Kevin speaks with James K. Steiner, the American orthopedic surgeon who designed the ATLS course after his family was involved in a tragic air accident. The program is both moving and inspiring, highlighting the importance of coordinated trauma care.
Meet the Speakers: Friends of St Emlyns
We are excited to reconnect with many friends of St Emlyns at the conference. Among the notable speakers are Mark Wilson, a renowned neurosurgeon from London, and Karen Brodie, a respected vascular and trauma surgeon. Ross Fisher, a pediatric surgeon from Sheffield, will be discussing pediatric trauma. Additionally, our colleagues from Sydney Hems, including Cliff Reed and Brian Burns, will also be presenting. The lineup reads like a who's who of UK and international trauma medicine, ensuring a wealth of knowledge and experience will be shared.
Our Mission at St Emlyns
At St Emlyns, we are dedicated to spreading trauma care education as widely as possible. None of our team members have any financial interest in the conference; our goal is purely educational. We hope to learn and share valuable insights with you, our community, to enhance our collective understanding and capabilities in trauma care.
Welcoming New Doctors to Emergency Medicine
This week is particularly special as it marks the arrival of new doctors in our emergency departments across the UK. This transition happens four or five times a year, bringing fresh faces, enthusiasm, and, understandably, a bit of nervousness. We urge everyone to extend kindness and support to these junior doctors. Our emergency departments thrive on a culture of learning and collaboration, and it’s essential to make our new colleagues feel welcome and valued.
If you are one of these new doctors, make sure to check out our induction blog posts and podcasts. They are available on the St Emlyns blog at stemlynsblog.org and on our iTunes podcast feed. These resources are designed to help you navigate the initial challenges and embrace the exciting journey ahead in emergency medicine.
The Importance of Continued Learning in Emergency Medicine
As we see from the current news, it’s a challenging time for UK emergency medicine. However, at St Emlyns, we are committed to bringing you the best resources, insights, and inspiration to help you continue delivering exceptional care to your patients. Our collaboration with the London Trauma Conference is just one example of our efforts to enhance the education and support available to all healthcare professionals in our community.
Conclusion
We are incredibly excited about this new venture and look forward to sharing our experiences and learnings from the London Trauma Conference with you. Whether you join us in person or follow along online, we hope this event will be as enlightening and inspiring for you as it promises to be for us.
Thank you for being a part of the St Emlyns community. Please continue enjoying your work in emergency medicine, and we’ll be back with more updates and insights very soon. Take care and thanks for listening!

Thursday Jun 26, 2014
Ep 6 - SMACC Back-Back on What to believe and when to change.
Thursday Jun 26, 2014
Thursday Jun 26, 2014
Navigating the Challenges of Early and Late Adoption in Medical Practice
In the ever-evolving landscape of medicine, the timing of adopting new treatments and technologies is a critical decision for clinicians. Simon Carley, in a discussion with Scott from St. Emlyn's podcast, delves into the complexities of being an early or late adopter, exploring the associated risks and benefits. This conversation highlights the fine line between innovation and patient safety, and the careful considerations required for responsible clinical practice.
The Risks of Early and Late Adoption
Both early and late adoption come with inherent dangers. Early adopters, eager to implement new innovations, may face unforeseen consequences. A historical example is the use of flecainide in the 1980s, initially believed to reduce ventricular disruptions in post-MI patients. However, it was later found to potentially cause more harm than benefit, underscoring the unpredictability of medical advances. On the other hand, late adopters risk failing to provide patients with the latest and most effective treatments, potentially resulting in suboptimal care.
Carley emphasizes the importance of a balanced approach, avoiding the pitfalls of both extremes. He discusses the concept of "dogmalacis," the enthusiasm for challenging established medical practices with new evidence. Both he and Scott agree that while it is essential to embrace new findings, clinicians must do so with caution and a thorough understanding of the current evidence base.
The Complexity of Determining Optimal Timing
Determining the optimal timing for adopting new practices—referred to as the "Goldilocks moment"—is complex and often only clear in hindsight. Carley notes that senior clinicians, in particular, must exercise careful judgment, understanding the strength of the evidence supporting current practices before making changes. This prudence is crucial to ensure that new practices are adopted based on solid evidence rather than mere enthusiasm.
Case Study: Targeted Temperature Management (TTM) Trial
The discussion includes a specific example: the Targeted Temperature Management (TTM) trial, which challenged previous beliefs about the benefits of hypothermia in post-cardiac arrest care. The trial suggested that fever avoidance was more critical than aggressive cooling, sparking significant debate. This case illustrates how new evidence can disrupt established practices and provoke emotional responses among practitioners.
Carley and Scott also discuss the need for rigorous evidence, particularly randomized controlled trials (RCTs), to support the adoption of new technologies and treatments. They highlight the glidescope trial, which demonstrated potential harm from the device in a randomized setting. The scarcity of such trials in evaluating new medical technologies points to a gap in evidence-based practice, stressing the importance of high-quality research to guide clinical decisions.
Balancing Innovation with Caution
Carley shares personal reflections on the challenges of balancing innovation with caution. While acknowledging the necessity of early adopters for medical progress, he stresses the need for careful consideration and expertise. Not every clinician or situation is suited for early adoption; it requires a deep understanding of the underlying science and a cautious approach to patient care.
He draws parallels between professional and personal experiences, noting his own tendency toward late adoption in certain areas, such as his decision to marry. This anecdote serves as a metaphor for the broader discussion, highlighting that timing in adoption is crucial and often a personal, context-dependent decision.
Embracing Continuous Improvement
The conversation culminates in a shared commitment to continuous improvement in medical practice. Both Carley and Scott emphasize the importance of doing the best with current knowledge and being ready to change when better evidence becomes available. They resonate with Maya Angelou's quote: "Do the best you can until you know better. Then when you know better, do better." This principle captures the essence of their discussion, advocating for a flexible and reflective approach to clinical practice.
Conclusion
Navigating the challenges of early and late adoption in medicine requires a careful balance between innovation and caution. Clinicians must be willing to embrace new evidence and change practices while ensuring that these changes are grounded in solid, high-quality research. The dialogue between Simon Carley and Scott highlights the complexities and responsibilities involved in this process, underscoring the need for continuous learning and adaptability in medical practice. Through thoughtful consideration and a commitment to evidence-based care, clinicians can optimize patient outcomes and advance the field of medicine.
